Health Practitioner Burnout, Safety Implications, and Programmatic Fixes: A Systematic Literature Review of Current Literature Reviews—200 Proof*
Abstract
High rates of workplace psychological stress and burnout have been chronic among Healthcare Practitioners. Research shows that Healthcare Practitioner psychological stress / burnout is related to poor quality of care and a high probability of making medical errors and mishaps resulting in harm to patients and even workers themselves. In response, relatively impactful programs have been developed to address Practitioner burnout. To derive a better understanding of the subject and inform best practices and policy regarding the problem and its fixes, this article reports findings from a novel study of a systematic (PRISMA-based) literature review of current (circa ~10 years <) literature reviews; or a distillation of reviews already at 100 proof then undergoing a further distillation into a review of 200 proof.* This study employed a grounded theoretic qualitative methodology to iteratively generate and enumerate descriptive themes from the study’s literature review articles. This article reports on what is currently known regarding the precipitants of Health Practitioner Burnout, Burnout itself, its relationship to Safety lapses and mishaps, and Programmatic Interventions (i.e., Fixes). The primary conclusion is that Health Practitioners are the foundation of healthcare organizations and key to quality care and management / leadership should be concerned for their wellbeing; and this article provides a general blueprint in terms of addressing burnout and safety. Study Limitations and Future research are also discussed.
Author Contributions
Copyright © 2025 Ralph J Johnson
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have no conflict of interest to declare.
Citation:
Introduction / Background
Considerable concern regarding Healthcare Practitioner burnout and related secondary mental distress (e.g., anxiety, depression, depersonalization, emotional exhaustion, disengagement, etc…) continues to be voiced.1, 2 Though the issue is complex and multi-faceted, research has reported widespread levels of burnout that are substantially higher for Health Care Practitioners than the general population regardless of demographic characteristics and other personal factors.2 For example, there are estimates of more than half the nurses working in the U.S. and one in ten worldwide experience burnout with other health professions more or less mirroring these rates.2, (also see 3, 4, 5, 6) Reports in the literature suggest that those in the healthcare field, in general, and frontline practitioners like nurses specifically, are particularly prone to burnout and psychological ill-health due to extraordinary workloads, emotional draining demands, and work conditions.1, 2, 4, 5, 6, 7, 8, 9
A paramount concern is that Healthcare Practitioners experiencing a high degree of psychological distress and burnout may be inattentive and prone to medical errors endangering patients and even themselves or co-workers.2, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 Compounding this concern are other healthcare organizational-level effects and astronomical costs of burnout such as disengagement and diminished productivity, intention to leave, turnover, attrition, and erosion of team morale. 2, 12, 15 Indeed, the problem of Healthcare Practitioner burnout, safety, and their fixes is so staggering that hundreds of peer-reviewed research studies have been published regarding various aspects. This then raises the question of how to best address the problem.1, 4, 5, 6, 7, 8, 10, 11, 13, 16, 17, 18, 19, 20, 21.
The subject of Healthcare Practitioner psychological stress, burnout, safety implications, and ameliorative interventions coincided with the advent and development of electronic medical literature repositories and databases such as PubMed, Cochranes, Psych Lit, Google Scholar, and Scopious—to name a few. 1, 2, 5, 8, 9, 10, 11, 12, 14, 16, 17, 18, 19, 20, 21 Their accelerated, comprehensive, and thorough literature search engines vastly enhanced the ability to conduct more comprehensive yet exacting and systematic reviews of the scholarly literature regarding the subject. 3, 6, 8, 10, 11, 15, 16, 18, 20, 21
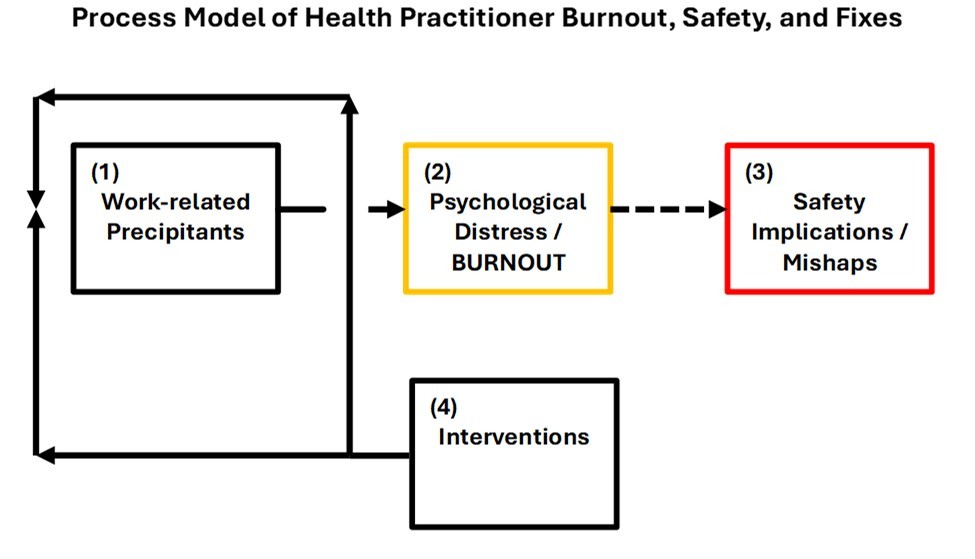
In order to provide a current and more formative grasp regarding the state of the research on the subject matter of Healthcare Practitioner psychological distress and burnout, safety implications, and corrective interventions, the intent of this article is to report findings from a novel study that conducted a theoretic grounded qualitative systematic 22 literature review of literature reviews in the past 10 years or less. The uniqueness of this study is there are so few systematic literature reviews on literature reviews in the scientific scholarly literature it is extremely difficult to pin down a number and they are not considered a category of review in the health field.23 This report considers the following components of the burnout, safety, and intervention “equation” in their logical sequence: (1) Contributing Work-related Precipitants; (2) Psychological Distress / Burnout; (3) Safety Implications / Mishaps; and (4) Interventions (see Process Diagram 1).
This diagram shows a process model of (1) the precipitants of Psychological Distress and Burnout leading to, (2) the condition of Psychological Distress / Burnout, which in turn leads to Safety mishaps. The dashed line depicts the tenuousness of that relationship between (2) and (3). And finally (4) depicts the Intervention Programs breaking the connection between (1) and (2) by addressing / disrupting the precipitant conditions necessary for Psychological Distress / Burnout to occur and at minimum reasonably containing them.
Method
The aim of a literature review of peer-reviewed literature reviews on Healthcare Practitioner burnout, safety, and its fixes is to create a further synthesis / purification of the scientific and best practices literature, or put differently, a further distillation from 100 proof into near-200 proof.* The hope was to highlight gaps in knowledge lending themselves to avenues for further inquiry and derive recommendations based on best practices to address the problem of increased burn-out and decreased safety in healthcare.
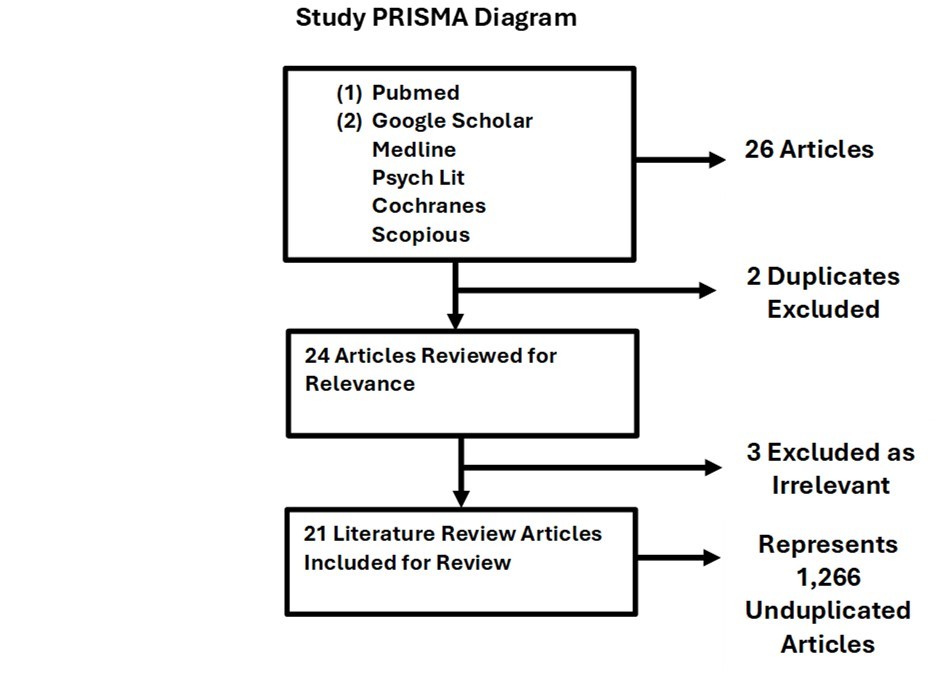
This review generally adhered to the guidelines for Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA).22 The search of the scholarly literature for reviews used Key Words, variants, and Booleans: “Healthcare Providers,” “Healthcare Workers,” “Burnout, Safety,” and “Literature Review.” Since the study focused on the current state of the science, the literature search was restricted to the past 10 years; moreover, only peer-reviewed and English or translated into English literature review articles were considered for inclusion. The primary search engine that was used was PubMed, followed with a cross-check, by Medline, Good Scholar, Psych Lit, Cochrane, and Scopious; until subsequent searches proved to be overlapping, further searches were halted. Since the study focused on the current state of the science, the literature search was restricted to the past 10 years; moreover, only peer-reviewed and English (or translated into English) literature review articles were considered for inclusion. Overlap was uncovered early on and duplicates were easily identified and pre-excluded except for two articles, which were caught in subsequent examination and removed. In further subsequent examination, three more were excluded because they were deemed irrelevant.
The literature search and examinations yielded 21 articles through the following systematic search and inclusion process (see Study PRISMA Diagram 2).
Initially, 21 articles would appear insignificant and possibly unrepresentative. However, the 21 articles—because they were literature reviews—actually represented an unduplicated count of 1, 266 peer-reviewed, scholarly, scientific, peer-reviewed articles related to various aspects of Healthcare Practitioner burnout, safety, and interventions. Nevertheless, some of the 21 articles did emphasize some aspects of burnout, safety and interventions more than others (see Article Different Emphases Table 1).
Table 1. Articles’ Different Emphases| Emphases | Count |
|---|---|
| Burnout | 11 |
| Safety | 12 |
| Interventions | 15 |
Table 1 shows that the literature review articles provided a general balanced coverage of the components of Burnout, Safety, and Intervention.
It should be noted, the articles overwhelmingly represent Western Nation Health Practitioners (see Table 2), though one in the Britain category included a Third World comparison.
Table 2. Articles’ National Origin| Nation of Origin | Count |
|---|---|
| Britain (contained 3rd World comparison) | 11 |
| USA | 6 |
| Scotland | 2 |
| Switzerland | 1 |
| Total | 21 |
Though there was some balance achieved regarding the general representation of Health Practitioners’ vocations, there was an evident bias towards one type of Healthcare Practitioner vocation, namely, nurses (see Table 3).
Table 3. Articles’ Health Practitioner Vocations Focus| Health Practitioners’ Vocations Focus | Count |
|---|---|
| Healthcare Workers (includes nurses) | 11 |
| Nurses (specifically) | 8 |
| Radiographers | 1 |
| Physicians / Dentists | 1 |
| Total | 21 |
It is not surprising that nursing and nurses would be overrepresented. More research has been done on nursing / nurses as they are of greatest concern, because their role is vital to the provision of healthcare and they are the frontline Healthcare Practitioners; therefore, they experience higher precipitating factors related to burnout and are in the position of making burnout-related inattentive critical safety mishaps. 13, 17, 18, 19, 21 However, other types of Healthcare Practitioners are more and less at risk as the literature search revealed.2, 5, 6, 8, 10, 12, 13, 14, 15, 20 Notably, overall. the articles derived in the search and inclusion appeared to provide a strong representation of the subject under study. This suggests that the findings from this study would be generalizable, and scientifically informed recommendations are advanced in the interest of best-practices.
A grounded 24, 25, 26 theoretic qualitative methodology was used to iteratively generate and assign themes to the study’s literature review articles (i.e., code), until thematic saturation, and an exhaustion of themes, was achieved. The inherent risk in this process is that some themes will be missed, but the assumption is that a general and credible assessment will be produced 25.
The penultimate aim of this process was to produce an integrated, synthesized end-product consisting of brief descriptive accounts of precipitants of burnout, the condition of burnout itself, consequent safety implications, and corrective interventions as well as a needs assessment on the state of effectiveness research.
Findings
Precipitant Factors Related to Psychological Distress / Burn-out
Nearly ubiquitously, the factors related to Healthcare Practitioner burnout were: high workloads, shift work, excessive work hours, schedule inflexibility, time pressures, communication overload and interruptions, value incongruence, low control over the job, low safety levels, negative and uncivil and toxic professional relationships and work / social environments, and poor leadership and unsupportive management.1, 4, 5, 6, 7, 9, 10, 15, 20 (also see 3). Any relations / effects from personal or demographic factors were mixed and slight to none.2, 8
Flynn et al.12 found that younger nurses were more prone to burnout, specifically due to not having developed resilience or sufficient situational coping skills. They suggested the counter-intuitive findings merited further investigation.14. Basu et al.5 observed that workplace stressors were primarily responsible for burnout that resulted in a high “intention to leave”; and noted that with high attrition the workplace situation only got worse for those remaining.(also see 7). Koontalay et al. 19 also found regarding the advent of the COVID-19 pandemic that inadequate preparedness and psychological distress (i.e., fear, anxiety, frustration, and stigma) increased substantially as a response to the pandemic, feelings of unpredictability, lack of resources and infrastructure, a perceived unsafe workplace, and lack of competent leadership or leadership’s support, and resulted in high levels of burnout in Healthcare Practitioners. They also noted frontline Healthcare Practitioners, which naturally would include a higher proportion of nurses, suffered more from the precipitants of burnout.10, 12, 13, 20
Sabitova, Hickling, Priebe3 found that working conditions—particularly hospital constraints, poor infrastructure, deficient equipment, lack of supplies and medications, especially in the Third World—were sources for poor morale (aka burnout). Additionally, poor financial and non-financial rewards (e.g., career development, advancement, teaching / learning), job security, and excessive workloads also were contributing factors to low morale and a potential for burnout.(also see 4) Elliott et al. 4 found that shift work across an array of health professions was related to poor sleep, exhaustion, and emotional exhaustion—precipitants for burnout.20
Bronkhorst et al.1 noted that a “good organizational climate” was significantly related to positive outcomes such as low psychological distress and burnout; logically, the opposite was the case. Specifically, they found that collegiality between Healthcare Practitioners, mutual co-worker support, and constant civil communications were the hallmarks of good organizational culture with less risk for distress and burnout.3 Flynn et al. 12(also see 4) observed that increased demands of acute care settings, such as in Emergency Departments or the Intensive Care Units, especially excessive communications and interruptions, severely worsened psychological distress and burnout.
Finally, Li et al.8 detected no difference in burnout levels according to Healthcare Practitioner demographics, experience, geography, and specialties, except in the case where there were slightly lower rates in advanced Health Practitioners and single Health Practitioners.2.
Psychological Distress / Burnout
Healthcare Practitioner Burnout (e.g., “low morale”, “occupational weariness”) has been depicted as emotional exhaustion, depersonalization, and decreased worker accomplishment deriving from constant and chronic psychological distress.2 Burnout has been reported at epidemic proportions among Healthcare Practitioners in the U.S. and worldwide.1, 2 Few demographic factors are significant; burnout’s source is rooted in work environment co-factors.2 Bronkhorst et al. 1 observed that is often accompanied by depressive symptoms and general psychological malaise / fugue. Li et al.8 characterized workplace burnout in the literature as evidence by emotional exhaustion, low sense of personal accomplishment, low self-esteem, cynicism, low professional efficacy, occupational stress, and poor sleep.4, also see 20
Di Ora et al.20 noted in the Health Practitioner literature the concept of burnout includes overlap between symptoms and outcomes. Work disengagement, intention to leave the job, job abandonment, early retirement, medical miscommunication, process errors and subsequent mishaps and accidents are sometimes considered surrogate measures of workplace burnout.20 They also found a high degree of Health Practitioner value incongruence with their jobs and incivility were signs of burnout. Worse, Elliott et al.4 found that burnout includes negative attitudes towards patient care and safety.
Safety Implications
Undeniably, Health Practitioner burnout unchecked has detrimental medical care quality and safety implications for patients, co-workers, and the Health Practitioners themselves; but the nature and the extent of that relationship is sketchy and questionable.5, 8, 9, 12, 2 According to Hall et al.9 higher Health Practitioner burnout significantly results in more medical errors. Research unequivocally has shown that Healthcare Practitioner burn-out related inattention increases the risk for medication errors, infection precaution non-observance, failure to recognize life threatening signs /symptoms and delayed reaction, missed patient falls, needle sticks, and other critical safety issues and risky harm scenarios, including mortality.2, 4, 8, 20 These burnout situations were not related to personal or demographic factors. 9 Hall et al.9 found a direct and consistent relationship between workload (i.e., substantial numbers of patients), burnout, poor quality of patient care, and a high number of medical mistakes, which were actually underreported due to the high workload.
Health Practitioner burnout by whatever means is significantly related to poor patient care and safety, though there may be more “near misses” than actual adverse events.9 Flynn et al. 12 found that Health Practitioner burn-out, when organization-wide, can contribute to an unsafer organizational climate creating a detachment from workload, incomplete safety procedures (especially infection control), and decreased patient engagement. Nevertheless, that link between burnout and safety is tenuous at best due to under-or-over-reporting: under reporting seemed the result of punitive measures for reporting; whereas, over-reporting seemed to be caused by rewarding or encouraging reporting.17 Ironically, Flynn et al. and Hall et al 8, 12 observed that the very act of reporting errors also can exacerbate burnout in Healthcare Practitioners. These findings have led some to conclude there is no direct correlative link between Health Practitioner burn-out and safety.8, 12, 17 The ambiguous nature and link of that supposed relationship warrants definitive prospective research.2, 8, 12
Another interpretation of Jun et al.’s2 and Flynn et al.’s12 mixed findings regarding major surrogate safety measures of burnout, specifically, near misses and intention to leave / leaving, suggest that Healthcare Practitioners are opting out of work situations conducive to poor mental health and burnout in the interest of patient care and safety. That is, ironically, intention to leave, leaving the job, and job abandonment actually may be a tribute to Healthcare Practitioners’ professionalism—if they are suffering burnout and prone to safety breaches—they would rather leave than risk the health and well-being of their patients and colleagues. This is worthy of further investigation.
Along with the permanent psychological harm of burnout to Healthcare Practitioners, Whitcombe, Cooper, and Palmer 15 identified other physical hazards resulting from burnout. such as cross-infection, manual hand injuries, slip-trip-and-falls, soft-tissue back injuries, chemical-substance-medication exposure, solo work and violent or abusive patients (especially for mental health workers6), and the most prominent dangerous medical work-related injury, namely, non-attentive needle sticks.1, 15 In sum, Healthcare Practitioner burnout adversely affects Health Practitioners, patients, health organizations, and society worsening safety, quality of care, and Health Practitioners’ commitment.2
Additionally, burnout was cited consistently as a cause for Health Practitioners intent to leave their jobs, leave, or abandon their jobs, and seek early retirement.2, 7, 12, 15, 20 This increases recruitment and training costs to health organizations, further increases workloads and risk of burnout for those remaining, and reduces morale and quality of patient care. Overall, the financial loss to the entire healthcare system is staggering.2
Intervention Programs (“the Fixes”)
Organizational Level Interventions
In a perfect world, ideally workloads would be lowered, organization / worker values forged congruently , consistent civility would be maintained in the workplace, flex schedules would prevail, shift work would be abolished, time pressures would be dissipated, work would be inherently interesting and rewarding, and Health Care Practitioners would be supported 100% by informed, stellar, altruistic leadership, while burnout levels would bottom out. Presumably, burnout-related safety hazards and harms would then just disappear. As improbable as that seems, research suggests that interventions that address , fix, or even just tweak one or more fundamental and “tangible” organizational aspects precipitating burnout, are very effective in decreasing burnout.5 However, they also may be unrealistic, impractical, and most likely unaffordable.3, 5 For example, research shows that Health Practitioner psychological distress, a precursor to burnout, can be greatly reduced simply by improving civility and communication in the workplace or scheduling better or reducing workloads even a little.21
Psychological-Level Interventions
Most psychologistic interventions designed to help fight Health Practitioner burnout fall under the theoretical rubric of Cognitive Behavioral Therapy (CBT), which is designed to replace negative thought patterns and behaviors contributing to psychological distress and burnout, rather than change workplace conditions.8 The two most prominent components are Mindfulness and Resilience.
Mindfulness
Mindfulness programs train Health Practitioners in groups over a period of time with the aim of increasing their ability to contemplatively pay attention and be “in the present moment” non-judgmentally to facilitate relaxation and calm the body and mind.10 Research has shown that these programs are effective in reducing Health Practitioners’ stress levels and improving their attention and concentration to minimize workplace safety mishaps.10
Resilience
These programs aim to improve Health Practitioners’ equilibrium under stress by training them to keep a sense of control and continue to forge onward positively despite adversity and emotional distress.17 Early research reported that web-based resilience burnout prevention / intervention programs significantly improved resilience to psychological distress / burnout, improved well-being, work engagement, and improved overall emotions on par with didactic in-person ones; however, these claims have since been hedged substantially.16, 17, 19 However, by reducing burnout psychologically, these programs may improve the safety of the health organization, while preserving the mental health and well-being of staff. also see, 18. Regarding the value of on-line resilience training in general, Henshall et al. 17 found its benefits to be convenience and accessibility, though the downside was that it failed to capture support in the workplace that seems crucial to warding-off burnout. This suggests that both online and in-person burnout programs have benefits depending on the target audience and situation; a multi-modality approach is probably optimal.
Regardless of theoretical underscoring of psychological interventions addressing burnout, what appears to work are interventions incorporating participative leadership, an organizational culture facilitating interdisciplinary teamwork with civility, and feedback that emphasizes the positive aspects of the work in a safe, supportive environment.16
Culture of Safety
An intervention that has shown great promise in terms of addressing burn-out and related safety mishaps is the eponymous implementation of a Culture of Safety.11 Though varied and complex, a major feature of it is advancing the quality of healthcare and reducing patient and worker harm through focusing and learning from events / incidents and translating that into best practices and policy involving staff support in the learning process.11 Research has shown that a functional culture can be replaced with a socially supportive one through teamwork aimed at improving safety and communication; this is psychologically beneficial to Healthcare Practitioners and crucial to reducing / eliminating psychological distress and burnout.11, 1 Since health organizations managers are directly involved in promoting safety and caring for workers, worker perception and attitudes improves.11 In a Culture of Safety, frontline workers are also considered leaders too, thus, their feelings over control of their work improves, and their self-efficacy improves—reducing psychological stress and burnout, while improving job satisfaction.11
Overall, research has shown that implementing a Culture of Safety results in dramatic drops in Health Practitioner attrition and improvements in attitudes; there are improvements in working conditions, since communication and collaboration improves as Healthcare Practitioners are involved in planning of safety and even staffing, which have been sore points resulting in burnout.11, 2, 4, 6, 8, 9, 12 Studies have shown that when frontline Healthcare Practitioners felt management supported them and were concerned for their well-being, there was a reduction of psychological stress, low morale, and burnout, and quality of patient care increased—by-products of a Culture of Safety. 1, 7, 11, 12. Most importantly, a Culture of Safety strives for value congruence between the organization and the Healthcare Practitioner, ultimately reducing Healthcare Practitioner psychological stress and burnout.
Note: In the literature, there was mention of a burn-out reduction intervention for a hospital Emergency Department consisting of aromatherapy combined with massage sessions over a 12-week period that resulted in a slight reduction in short term anxiety levels. Also, the final verdict on Mentorship programs is that they do not affect workplace psychological distress and burnout.5
Discussion / Conclusion
This article provided a firmer grasp on the current state of science and best practices regarding Healthcare Practitioner burnout precipitants, actual burnout, safety implications, and corrective interventions through a theoretical grounded literature review of literature reviews on an extensively researched subject. Healthcare Practitioners play a fundamental role in quality of care and safety and are the foundation of healthcare organizations—hence, management / leadership should be concerned for their wellbeing. Poor healthcare work environments create psychological distress and burnout in Healthcare Practitioners, specifically, environments characterized by excessive workloads, shift work, value incongruence, low control over the job, inordinate time pressures, communications overload, incessant interruptions, negative / uncivil professional relationships, a toxic social climate, and uninvolved, uncaring, unsympathetic, and unsupportive management. The mental condition of burnout renders the Health Practitioners prone to making inattentive medical errors that place patients, co-workers and even themselves in jeopardy and harm. Fundamental Organizational fixes addressing the precipitants of Health Practitioner burnout, though very powerful, can be impractical and unaffordable. There are also impactful Psychological Intervention programs aimed at addressing and ameliorating the psychological distress and burnout itself through: Cognitive Behavioral Mindfulness and Resilience Training. Also, in a Culture of Safety there is a promising powerful multi-faceted and complicated intervention. Singularly, in combination, or with Fundamental Organizational fixes, they have been shown to be extremely powerful remedies in reducing Health Practitioner psychological distress and burnout.
What seems to make these Psychological Interventions work are the aspects they have in common, specifically: they are training and learning programs that emphasize teamwork and common purpose, management / leadership’s involvement and support / concern / caring, workers assuming a degree of control over their jobs, related job condition improvement, cohesive positive interdisciplinary communications, mutual professional respect and civility, and overall consciousness raising in terms of psychological distress and burnout avoidance.
There are vetted programs available to help Health Practitioners and health organizations improve workplace mental health in the interest of quality patient care and safety as well as worker well-being and safety.
Limitations
There was a discordance between the methodology of grounded iterative thematic enumeration of all variants and the aim of the study to produce a purer synthesis of already synthesized materials.24, 25, 26 Nevertheless, the method ensured a comprehensive identification, organization, and solid descriptive accounting of what is currently known, and the state of the science and best practices regarding the study’s subject matter. Another inherent limitation of the grounded methodology is the possibility of some extreme obscure variant escaping detection or being overlooked.25, 26 Nevertheless, the final product represented a staggering number of original peer-reviewed research study reports and probably nearly exhausted variants. Although this study only included peer-reviewed articles, missing the “grey” literature reviews (e.g., in-house program evaluations or trade journal articles), there was a degree quality control assurance regarding findings in terms of scientific merit. Another methodological limitation was that, as the study was a descriptive / qualitative inventory and not quantitative, findings were given equal weight; so there could be no effect size comparisons.14. Future research should consider meta-analysis. Similarly, there was no formal estimate of the quality of research articles included. Nevertheless, 16 of the 21 studies (77%) specifically adhered to PRISMA guidelines ensuring literature review quality.
It would be expected that restricting the key words for search articles would exclude journals using synonyms or foreign journals using different words; but this did not appear to be the case, as there was diversity of different terms and different nations from which articles came. Though most articles did come from the Western world, they represented a variety of Western nations, and even a Third World comparison nation was included in one of the journal articles. Of course, there is the issue to limiting the reviewed articles’ language to either English or translated English. Future research should similarly explore non-English speaking literature reviews as a comparison. Furthermore, treating Health Practitioners in the aggregate created a lack of heterogeneity, making generalizability to sub-groups difficult, but not impossible. This is another area that could benefit from future research. However, recent research reports indicate that all Health Practitioner sub-groups are more or less similarly affected by burnout and are at risk for making medical mistakes, and could benefit from programmatic interventions. 1, 4, 5, 6, 9, 11, 18
Recommendations / Future Research
Probably the most profound recommendation derived from this work is that, before a healthcare workplace plunges in a downward spiral and that devolves into an overwhelming morass of Health Practitioner burnout and related problems, leadership / management must act quickly and follow the scientific research based best practice blueprint contained in this research report and reach for that near “200 proof.”* Preventive intervention is generally less expensive than curative remediation.
Besides gaps in knowledge already identified in this review, other similar systematic literature reviews should be conducted on other high stress occupations where safety is a premium as a comparison to verify the universality of this study’s findings. For the same reason, cross-national literature review studies of literature reviews should be conducted too.
*Note: “Moonshiners” commonly refer to double-distilled near 200 proof spirits in common parlance as “White Lightening.” 27
Declarations
Ethical approval and consent to participate
Non-applicable, this was a commentary accompanied by a review of supporting open-source documents.
Consent for Publication
Yes.
Availability of data and materials
Yes, publications and sources are available on-line or provided or by author upon request.
Competing interests
None declared.
Funding
The author gratefully acknowledges UT-MDACC for in-kind support.
Authors’ Contribution
Non-applicable, there is one sole Author.
Acknowledgements
The Author wishes to gratefully acknowledge in-kind support of the Department of Lymphoma and Myeloma, UT-MD Anderson Cancer Center, Houston, TX. in the preparation of this manuscript. Also, the author thanks Mr. Jasper Olsem for the concept and his encouragement in pursuing the subject matter. The author also expresses appreciation Ms. Aileen “Acey” Cho freelance-copy editor for proofing and copyediting drafts. The opinions expressed are solely those of the Author. Reprints and correspondence should be addressed to the author at [email protected] or, UT-MDACC, Dept. of Lymphoma / Myeloma, Unit 429, 1515 Holcombe, Houston, Texas, 77030-400, U.S.A.. (832-372-3511)
References
- 1.Bronkhorst B, Tummers L, Steijn B, Vijverberg D. (2015) Organizational climate and employee mental health outcomes: A systematic review of studies in health care organizations.Health Care Manage Rev.40(3):. 254-71.
- 2.Jun J, Ojemeni M M, Kalamani R, Tong J, Crecelius M L. (2021) Relationship between nurse burnout, patient and organizational outcomes:. Systematic review.Int J Nurs Stud.2021; 119: 103933. doi: 10.1016/j.ijnurstu.2021.103933. Epub PMID: 33901940.https://www.sciencedirect.com/science/article/abs/pii/S0020748921000742?via%3Dihub .
- 3.Sabitova A, Hickling L M, Priebe S Job. (2020) morale: a scoping review of how the concept developed and is used in healthcare research.BMC Public Health. 20(1), 1166-10.
- 4.Elliott J, Hodges C, Boots M, Pattinson R, Gillen E et al. (2024) Mixed shift rotations, sleep, burnout and well-being in professions similar to radiographers: A systematic review.Radiography (Lond).2024;30(4): 1194-1200. doi: 10.1016/j.radi.2024.05.016. Epub. 38901073-10.
- 5.Basu S, Qayyum H, Mason S. (2017) Occupational stress in the ED: a systematic literature review.Emerg. PMID: 27729392.https://emj.bmj.com/content/34/7/441.long , Med 34(7), 441-447.
- 6.Johnson J, Hall L H, Berzins K, Baker J, Melling K et al. (2018) Mental healthcare staff well-being and burnout: A narrative review of trends, causes, implications, and recommendations for future interventions.Int. PMID: 29243348.https://onlinelibrary.wiley.com/doi/10.1111/inm.12416 , J Mental Hlth 27(1).
- 7.Świtalski J, Wnuk K, Tatara T, Miazga W, Wiśniewska E et al. (2022) Interventions to Increase Patient Safety in Long-Term Care Facilities-Umbrella Review.Int J Environ Res Public Health. 19(22), 15354-10.
- 8.Li L N, Yang P, Singer S J, Pfeffer J, Mathur M B et al. (2024) . Nurse Burnout and Patient Safety, Satisfaction, and Quality of Care: A Systematic Review and Meta-Analysis.JAMA Network Open.7(11):e2443059. doi: 10.1001/jamanetworkopen.2024.43059. PMID: 39499515.https://pmc.ncbi.nlm.nih.gov/articles/PMC11539016/ .
- 9.Hall L H, Johnson J, Watt I, Tsipa A, O'Connor D B. (2016) Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. PLoS One. PMID: 27391946https://pmc.ncbi.nlm.nih.gov/articles/PMC4938539/ 11(7), 10-1371.
- 10.Botha E, Gwin T, Purpora C. (2015) The effectiveness of mindfulness-based programs in reducing stress experienced by nurses in adult hospital settings: a systematic review of quantitative evidence protocol.JBI Database System Rev Implement Rep. 13(10), 21-9.
- 11.Finn M, Walsh A, Rafter N, Mellon L, Chong H Y et al. (2024) Effect of interventions to improve safety culture on healthcare workers in hospital settings: a systematic review of the international literature.BMJ Open Qual. 13(2), 10-1136.
- 12.Flynn C, Watson C, Patton D, O'Connor T. (2024) The impact of burnout on paediatric nurses' attitudes about patient safety in the acute hospital setting: A systematic review.J. Pediatr Nurs.2024;78: 82-89. doi: 10.1016/j.pedn.2024.06.023. Epub 16, 39019737-0882.
- 13.Hill B. (2017) Do nurse staffing levels affect patient mortality in acute secondary care?. , Br J 26(12), 698-704.
- 14.Stevanin S, Palese A, Bressan V, Vehviläinen-Julkunen K, Kvist T. (2018) Workplace-related generational characteristics of nurses: A mixed-method systematic review.J. Adv Nurs.2018 Jun;74(6): 1245-1263. doi: 10.1111/jan.13538. Epub PMID: 29424038.https://onlinelibrary.wiley.com/doi/10.1111/jan.13538 .
- 15.Whitcombe A, Cooper K, Palmer E. (2016) The relationship between organizational culture and the health and wellbeing of hospital nurses worldwide: a mixed methods systematic review protocol.JBI Database System Rev Implement Rep.14(6):. PMID: 27532655.https://journals.lww.com/jbisrir/fulltext/2016/06000 the_relationship_between_organizational_culture.13.aspx 103-16.
- 16.Härkänen M, Pineda A L, Tella S, Mahat S, Panella M et al. (2023) The impact of emotional support on healthcare workers and students coping with COVID-19, and other SARS-CoV pandemics - a mixed-methods systematic review.BMC Health Serv Res.23(1):. 751, 10-1186.
- 17.Henshall C, Ostinelli E, Harvey J, Davey Z, Aghanenu B et al. (2022) . Examining the Effectiveness of Web-Based Interventions to Enhance Resilience in Health Care Professionals: Systematic Review.JMIR Med Educ.8(3):e34230. doi: 10.2196/34230. PMID: 36066962.https://pmc.ncbi.nlm.nih.gov/articles/PMC9490530/ .
- 18.Di Nota PM, Bahji A, Groll D, Carleton R N, Anderson G S. (2021) Proactive psychological programs designed to mitigate posttraumatic stress injuries among at-risk workers: a systematic review and meta-analysis. Syst Rev .10(1): 126. doi: 10.1186/s13643-021-01677-7. PMID: 33910641 PMCID: PMC8079856 DOI: 10-1186.
- 19.Koontalay A, Suksatan W, Prabsangob K, Sadang J M. (2021) Healthcare Workers' Burdens During the COVID-19 Pandemic: A Qualitative Systematic. 10.2147/JMDH.S330041. eCollection 2021. PMID: 34737573 PMCID: PMC8558429 DOI: , Review.J Multidiscip Healthc 14, 3015-3025.
- 20.Dall'Ora C, Saville C, Rubbo B, Turner L, Jones J et al. (2022) Nurse staffing levels and patient outcomes: A systematic review of longitudinal studies.Int. J Nurs Stud.Oct;134: 104311. doi: 10.1016/j.ijnurstu.2022.104311. Epub PMID: 35780608.https://www.sciencedirect.com/science/article/pii/S0020748922001407?via%3Dihub .
- 21.Silva J A, Mininel V A, Fernandes Agreli H, Peduzzi M, Harrison R et al. (2022) Collective leadership to improve professional practice, healthcare outcomes and staff (well-being).Cochrane Database of Systematic Reviews. Issue 10. Art. No.: CD013850. DOI: 10.1002/14651858.CD013850.pub2.https://pmc.ncbi.nlm.nih.gov/articles/PMC9549469/pdf/CD013850.pdf .
- 22.Page M J, McKenzie J E, Bossuyt P M, Boutron I. (2020) statement: an updated guideline for reporting systematic reviews.BMJ. The PRISMA .
- 23.Paré G, Kitsiou S. (2016) Chapter 9 Methods for Literature Reviews inHandbook of eHealth Evaluation: An Evidence-based Approach [Internet]. (Eds Francis Lau and Craig Kuziemsky).
- 24.Glaser B G. (1967) and Strauss AL.The Discovery of Grounded Theory: Strategies for Qualitative Research.Aldine Transaction;. , New Brunswick
- 25.Strauss A. (1998) Corbin J.Basics of qualitative research– techniques and procedures for developing grounded theory, second edition.London: Sage Publications;.