A Qualitative Assessment of an Innovative Suicide Prevention and Treatment Approach: Contextual-Conceptual Therapy
Abstract
Mental health and mental illness is a critical to a person’s overall health. In the United States alone, mental illness effects one in six adults. Furthermore, 40% of those individuals who die of suicide have been diagnosed with a mental health condition or illness. Yet, there is a paucity of research on innovative methods that help prevent suicide.
The Contextual-Conceptual Therapy (CCT) approach introduces an innovative way to treat suicide by working to uncover the strengths of the suicidal person and addressing a person’s true self. The CCT approach was developed over the course of 25 years working with more than 16,000 suicidal patients in Seattle, Washington, and is tailored specifically for primary and secondary prevention of suicide. While there has been anecdotal evidence of the effectiveness of the CCT program, the program has yet to be formally evaluated. This qualitative research study aims to understand the impact the CCT approach has had on its clients. Eleven former CCT clients were recruited to participate in semi-structured interviews. Outcomes described by participants included an increase in curiosity and self-efficacy as a means through which to decrease suicide ideation and behavior, and proved to be incredibly powerful in changing long-term outcomes.
This qualitative study is a first-step in providing critical insight on suicide prevention for wider dissemination. At a time when adverse mental health and illness is impacting the lives of millions of people, the CCT approach has the potential to address suicide, mental illness and mental health across diverse populations.
Author Contributions
Academic Editor: Bhalchandra Mirlekar, Postdoctoral Research Associate Ph.D., National Center for Cell Science (NCCS), India.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2020 Amita Vyas, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
This manuscript has not been published elsewhere and is not under submission elsewhere.
There is no conflict of interest, or alternatively, disclosing any conflict of interest that may exist.
Citation:
Introduction
Mental health is one’s emotional and psychological state and although it is not the same as mental illness, poor mental health can lead to both mental and physical illnesses. Mental illness refers to a wide range of disorders that affect mood, thinking and behavior and can be caused by biological factors such as genes or brain chemistry, trauma and abuse, and family history of mental illness. It is without question that both adverse mental health and mental illness continue to be regarded as public health priorities in the United States and globally, with significant short and long-term consequences to an individual’s physical health and happiness, as well as a nation’s prosperity. Further, suicide and suicide ideation, which stem from both poor mental health and mental illnesses, continue to be a pervasive problem in the United States, impacting all dimensions of health, including economic, social, and cultural 1. In 2002, suicide was the fourth leading cause of death for adults between the ages of 18 and 65 years with approximately 25,000 suicides for this age group in the United States 2. Unfortunately, age-adjusted suicide rates increased in the U.S. by 33% between 1999 and 2017; this is the highest rate since at least 1975, and in 2017 approximately 47,000 suicides occurred 3. Further, a 2018 Centers for Disease Control and Prevention (CDC) report illustrated recent declines in life expectancy in the U.S., and partially attributed this decrease to suicide at young ages along with increases in other leading causes of death 4. In 2016, nearly 45,000 suicides occurred, among whom 54% did not have a prior known mental health condition 5. From an economic perspective, a 2013 CDC report which included lower rates of suicide when compared to 2017, calculated suicide as a $50.8 billion cost for fatal injury. This includes medical and work loss costs of the fatal injury 6.
Suicide is complicated in that there is not one single determining factor. Risk of suicide has been shown to be higher in those who have lost someone close to them from suicide (i.e. family member, co-worker, etc.) or have a substance-use disorder 7, 8. Furthermore, research has shown that when media highlights suicide or details uninformed suicide reports, it can contribute to increased suicide rates 7. It is important to note that attempted suicide is one of the strongest risk factors for completed suicide in adults 9. It is estimated that individuals who attempted suicide were 38 to 40 times more likely to commit suicide than those who had not attempted suicide 10. In 2017, 10.6 million adults aged 18 or older reported having serious thoughts of suicide, also known as suicide ideation, and 1.4 million adults made a non-fatal suicide attempt in the past year 11.
Suicide Prevention and Treatment Interventions in the U.S.
In the last decade, various primary and secondary suicide prevention approaches have been utilized to combat the increase in number of suicide related deaths. These include gatekeeper trainings; school-based programs; hotlines; screening programs; cognitive behavioral therapies and medication, and all with varying levels of success. It is imperative that evidence-based programs are adapted and scaled, and new approaches and methods must be developed and tested.
Gatekeeper interventions involve community trainings to identify people who are at risk for suicide and then provide referrals for appropriate resources 8. It has been posited that social support can be effective at addressing both individual and social factors associated with suicide-risk. While social support strategies like gatekeeper trainings were found to have positive impacts on decreasing depressive symptoms for those with suicide ideation, these results have been mixed and inconsistent 12. School-based interventions for suicide prevention are common since often mental health disorders begin in childhood or adolescence 13. It has been posited that interventions that focus on mental health literacy, risk awareness, and skills may decrease suicide attempts among students 12. However, only a few randomized control studies (RCTs) have been conducted and while some found improved knowledge and attitudes towards suicide, there was no actual effect on suicidal behavior, and other studies found mixed outcomes with respect to suicidal behavior 14, 15, 16, 17, 18, 19, 20, 21.
Crisis hotlines are intervention services for more imminent risk. Most notably, the National Suicide Prevention Lifeline (NSPL) was created by the Substance Abuse and Mental Health Service Administration (SAMHSA) of the U.S. Department of Health and Human Services. In times of unexpected increased volume however, crisis centers struggle to answer each call that is placed due to their limited capacity. For example, after the death of actor Robin William’s by suicide, calls placed to the NSPL increased by up to 300% to almost 13,000 calls, and yet “calls answered” decreased from an average of 73% to 57% 22. This is an example of how high profile events have the potential to influence norms, and increase utilization of hotlines and other services.
Prevention efforts in the healthcare setting via appropriate screenings, have also become more common over the years. “Zero Suicides” operates under the belief that suicides for people in the healthcare setting should and must be preventable. However, screenings for mental health and illness do not always occur consistently and continuously, especially within systems that don’t have a comprehensive and holistic definition of health and healthcare. The program’s goal is to address systems in the healthcare setting that create gaps in care for people with suicide ideation. The initiatives include routine screening for suicide at different points in the healthcare journey, designing safety crisis plans, and treating suicide directly as opposed to treating underlying mental illness or substance use disorders 8. While there have been some successes with specific screening programs, the evidence has been largely inconclusive in determining how beneficial screenings are in regards to the prevention of suicide attempts 23.
The National Institute of Mental Health (NIMH) indicate medication and psychotherapy as the primary treatment options for people with suicide ideation by addressing underlying symptoms of depression and anxiety that often accompany suicidal thoughts and behaviors 2. Cognitive Behavioral Theory (CBT) and its derivative therapies are the most common forms of psychotherapy in the suicide prevention and treatment literature. This theory, adopted by the early work of by Aaron T. Beck and Albert Ellis, posits that maladaptive thought processes, such as certain beliefs about the world, the self, and the future, lead to emotional distress and behavioral issues by creating harmful, automatic thought patterns 24. CBT aims to use therapeutic strategies to change these maladaptive thought processes. CBT is a commonly used therapeutic approach for suicide prevention, however, the strongest observed efficacy for this type of treatment approach exists for issues related to anxiety disorders, somatoform disorders, bulimia, anger control problems and general stress rather than for suicide prevention 24.
Dialectical Behavioral Therapy (DBT), a specific type of CBT, has been found to have varied success in reducing suicide ideation and behaviors in adolescents 12 where therapists encourage clients to strive for a balance between acceptance of circumstances outside of one’s control with striving for adaptive behavior changes 25. While often used to treat personality disorders 25, DBT has been found to be effective in reducing suicide ideations and behaviors in adolescents 12, however, more so among adolescents with or suspected to also have borderline personality disorder or bipolar disorder 26.
Empirical evidence of programs that effectively prevent primary or repetition suicide attempts is limited. Although several studies support the efficacy of cognitive behavioral therapy or problem-solving therapy for reducing suicide behavior, there has been a lack of newer and more innovative prevention methods, and given the increases in suicide attempts and deaths, the need to identify, evaluate, and disseminate new programs is paramount. The present qualitative study was aimed at describing a new approach to suicide therapy, the CCT model, and to examine its potential in yielding impact for its clients. This formative study is an important step in designing a future randomized controlled trial to quantitatively assess outcomes of this new and creative approach.
Materials and Methods
Participants and Procedures
The Contextual-Conceptual Therapy (CCT) approach was developed by a suicidality expert working in Washington state whose aim was to fully understand a suicidal person’s core experience by exploring the language they use while in the midst of their suicidal crises. CCT is founded in the notion that a suicidal person’s own language and feelings are actually an expression of an identity crisis. CCT uses maps, models, and metaphors to guide the suicidal person to the root of their suicidal thinking and to an intimate level of self-knowledge 27. The CCT approach argues that individuals with chronic suicide ideation are experiencing an identity crisis between the “bad” person they believe they are and try not to be, and the “good/perfect” person whom they strive to be. This disconnect at the individual-level creates severe distress within the minds of suicidal individuals to the point where they feel like the only way to escape the psychological pain is to kill themselves. The approach encourages the consideration of the metaphoric language that participants use to express their feelings as a way to engage their creative mind and destabilize the logic behind their reasons for suicide. Through the exploration of being stuck, trapped, or lost, and by focusing on their language, the therapist can help unearth unconscious yearnings and understand with what they are truly struggling with. While other psychotherapeutic strategies attempt to stabilize a suicidal person and their suicidal thoughts, the CCT approach posits that this strategy can be harmful and temporary since providers are treating this false-self unconsciously created while a person is in this bifurcated state, as opposed to addressing the true-self which consists of neither of these identities. Through de-stabilizing the person with suicide ideation, CCT aims to help people find new insight into the true context in which they exist each day and to flourish as their true selves. A more detailed description of the CCT program may be found at http://www.suicidetherapy.com/.
The CCT model was developed over the course of 25 years working with more than 16,000 suicidal patients in Seattle, Washington, and is tailored specifically for primary and secondary prevention of suicide which is unique to behavioral therapies that have been studied previously and found to be efficacious. Further, while other cognitive therapy models aim to correct maladaptive thinking and behaviors, the CCT approach works to uncover the strengths of the suicidal person, and does not aim to fully replace other therapies but can also function as a precursor to enhance the effectiveness of other interventions. Potential CCT clients complete an initial 20-minute phone screening that assesses their history of therapies and interventions and current/previous suicide ideation and behavior. While the length of the program varies depending on the need of the individual, the program typically lasts three months, which includes a weekly, two-hour session. Sessions are typically one-to-one, however at times, a family member may be invited to participate. In between sessions and throughout the course of the program, participants receive tailored homework assignments. Clients complete the program once the CCT therapist and client agree that their thinking is more future-oriented, and they have an absence of suicidal thinking. Anecdotal evidence suggests that the CCT program is a highly effective suicide prevention program; however, to date there have been no formal evaluation study to assess the outcomes of this program.
The present data is derived from qualitative interviews (n=11) that were conducted with a purposive sample of male and female adults over the ages of 18 who had completed the CCT program in Washington state. Former clients of the CCT program were offered the opportunity to participate in semi-structured interviews and a recruitment email was sent to adult clients who had finished the program in the last 24 months. All interested persons were sent an electronic version of the consent form to review prior to speaking to a member of the study team, and verbal consent was obtained at the time of the scheduled interview. Sixty-minute, one-on-one in-depth qualitative interviews were conducted and recruitment ended after 11 interviews when it appeared that an adequate level of saturation had been reached. The interview guide consisted of questions asking participants about their perceptions surrounding the CCT approach and its activities, as well as their perceived impact of the program. Participants were encouraged to freely express their opinions and provide specific examples of their experiences. Interviews were conducted via WebEx and were audio recorded and transcribed for analysis. Following the interviews, a brief survey was sent out to study participants to obtain basic demographic information including race/ethnicity, family status, and level of education. Table 1 describes characteristics of the study sample. All procedures for this study, including protection of human subjects, were reviewed and approved by the Institutional Review Board (IRB) at the GW Office of Human Research (IRB ##NCR191356).
Table 1. Characteristics of the Study Population| Characteristics | N (%) | |
| Gender | Male | 7 (63.6) |
| Female | 4 (36.4) | |
| Age | 25-44 | 5 (45.5) |
| 45-64 | 4 (36.4) | |
| 65+ | 2 (18.2) | |
| Ethnicity | Hispanic | 0 (0.0) |
| Non-Hispanic | 8 (100.0) | |
| Race | White | 7 (87.5) |
| Other | 1 (12.5) | |
| Current Marital Status | Married | 2 (25.0) |
| Not married | 6 (75.0) | |
| Has Children | Yes | 3 (37.5) |
| No | 5 (62.5) | |
| Highest Level of Education Completed | Less than 1 year of college | 2 (25.0) |
| 1 year or more of college | 6 (75.0) | |
| Time Since CCT Program | Less than 1 year | 5 (45.5) |
| 1 year or more | 6 (54.5) | |
| Length of Time in CCT Program | Less than 1 year | 4 (36.4) |
| 1 year or more | 7 (63.6) | |
| Has Received Previous Mental Health Treatment | Yes | 11 (100.0) |
| No | 0 (0.0) | |
| Presenting Mental Health Issue | Suicide, Ideation and/or Attempts | 6 (54.5) |
| Substance Use | 2 (18.1) | |
| Anxiety | 1 (0.1) | |
| Depression | 4 (36.3) | |
| Grief | 2 (18.1) | |
| Other | 3 (27.2) |
Measures
The following variables and constructs were identified in each transcript.
CCT Client Characteristics
a. Previous mental health treatment experiences including the type of interventions clients have been through and their perceptions of those experiences.
b. Readiness as defined by a client’s willingness and motivation to participate in all portions of the CCT program.
CCT Therapist Characteristics were Defined by Being a Guide, Teacher, Friend, Parent-figure and Having an “Outlandish” Personality.
a. A therapist as a guide for the participant’s journey while in the program.
b. A therapist as a teacher who is sharing CCT knowledge and theory.
c. A therapist as a friend with whom there is a trusting relationship outside that of a typical therapist.
d. A therapist who is a parental figure and is a role model and a trusted person in the participant’s life.
e. A therapist who has an “outlandish” personality that is atypical, especially when compared with past experiences with a therapist.
CCT Program Activities
a. Referrals: how the client learned about the CCT program.
b. In-session exercises: specific exercises that clients noted that occurred during their one-on-one time with the CCT therapist.
c. Props: physical posters, models, and figures used by the CCT therapist.
d. Homework: exercises that the clients did outside of their one-on-one time
e. Creative activities: writing, reading, or other activities that required participants to think creatively rather than logically.
f. Family sessions: having a family member attend a session and includes their perceptions of that experience.
CCT Program Characteristics
a. Novel approach: noting how unique and different the CCT approach is compared to previous therapies and interventions.
b. Use of metaphors: talking about specific examples of metaphors and how these assisted and supported them.
c. Chaotic: describes the non-linear or unusual direction, and this may refer to an individual session or an individual’s experience as a whole.
d. Address root causes: understanding the core issues that for an individual’s mental/emotional state and suicide ideation.
e. Long-term impact: whether the knowledge that a client has learned still resonates with them, or if they still practice skills that they learned.
f. Barriers: struggles or issues that prevented someone from participating in all or part of the CCT program.
CCT Program Outcomes
a. Mindset transformation: When a client starts to notice their ability to fully grasp the knowledge of what the CCT program has taught them.
b. Curiosity: newfound desire or interest to explore new concepts whether it be about the world or oneself.
c. Empowerment/self-efficacy: Feeling confident in one’s ability to make decisions about their life.
d. Coping behaviors: strategies that clients use to maintain their newfound state of mind.
Analysis
Using a preliminary coding scheme, six trained research assistants coded the first four interview transcripts separately and then compared results. After working through the initial transcripts, the coding scheme was revised to the final measures documented above in order to more accurately reflect the purpose of this study. Once the final coding structure was decided upon, only one researcher coded the remaining interviews in an attempt to minimize biases from multiple researchers coding different transcripts. The final database quantified how often each variable was coded, as well as unique quotes or common themes that stood out from the interviews.
Results
To elicit a thorough assessment of each interview transcript, a percentage of codes within each domain was calculated to reflect how often these concepts were mentioned during interviews, and verbatim quotes were extracted to further illustrate each domain. Table 2 provides the overall frequencies and percentages of each construct.
Table 2. Overall frequencies and percentages of specific constructs| Domain | Construct | N (%) |
|---|---|---|
| CCT Client Characteristics | Previous mental health treatment experiences | 40 (71.4) |
| Readiness | 16 (28.6) | |
| CCT Therapist Characteristics | Guide | 17 (65.4) |
| Teacher | 2 (7.7) | |
| Friend | 3 (11.5) | |
| Parental-figure | 2 (7.7) | |
| Outlandish persona | 2 (7.7) | |
| CCT Program Activities | Referral | 11 (16.4) |
| In-Session Activities | 14 (20.9) | |
| Props | 12 (17.9) | |
| Homework | 13 (19.4) | |
| Creative Activities | 10 (14.9) | |
| Family Sessions | 7 (10.4) | |
| CCT Program Characteristics | Novel approach | 22 (30.1) |
| Use of metaphors | 11 (15.1) | |
| Chaotic | 7 (9.6) | |
| Address root causes | 12 (16.4) | |
| Long-term impact | 14 (19.2) | |
| Barriers | 7 (9.6) | |
| CCT Program Outcomes | Mindset transformation | 13 (24.1) |
| Curiosity | 16 (29.6) | |
| Empowerment/Self-Efficacy | 15 (27.8) | |
| Coping behaviors | 10 (18.5) |
CCT Client Characteristics/Sample Characteristics
(Table 1) below presents the sociodemographic characteristics of study participants. Of the eleven participants, 64% (N= 7) were male and 36% (N=4) were female, and the majority of clients (55%) had completed the CCT program less than a year ago. Eight-eight percent of the participants were White, and 75% had one or more years of college education. The majority of participants (55%) reported seeking out CCT for suicide ideation or attempts, with the second most common mental health issue being depression (36%).
All participants had previous experiences with mental health treatment. Study participants’ previous experiences with mental health therapies and programs accounted for 13.0% of all codes and 71.4% of codes for client characteristics. Previous treatments included psychiatric hospitalizations, individual CBT and DBT sessions, and pharmaceutical interventions. For all the participants these programs either did not provide relief from their symptoms, or they only provided temporary relief and/or short-term coping strategies. One participant noted the following regarding their past therapy experiences:
“ So I have been in therapies since I can remember, maybe 7 or 8 years of age. I have been institutionalized. I have been through counselors, family counselors, yeah so I would say that on and off for pretty much my whole life. Never really finding success, sort of just finding a way to function, if that’s the right word. To be alive but not necessarily living. ...finding new therapies would invigorate and allow me to tread water longer and then eventually still just sort of tire you out and you end up returning back to the system, being on various medications constantly.” ( Female, 25-44)
Another Participant Stated
“So um, so my kinda mental health history in that regard is I did pretty much all the previous kinds of therapies like you know talk therapy, CCD, CBT, and the such. I had private therapists, psychiatrists, and was also in group settings. I kinda did a little bit of everything um before. But nothing worked.” ( Male, 25-44)
Participants also discussed the importance of readiness and noted being ready and willing to participate in program activities was crucial to their success with the program. One participant stated:
“I would say that ( readiness ) would be a key element. I think part of this program is your own willingness to do your own work a little bit, and talking about these things, and being frustrated.” (Female, 25-44).
CCT Therapist Characteristics
Across all interviews, participants spoke highly of their CCT therapist and their tone was often endearing and incredulous. The CCT therapist was most often described as a guide (65.4% of codes), and a teacher (7.7% of codes). This sentiment differed from descriptions of previous therapists who took a more prescriptive approach. One participant noted:
“It definitely felt like ( the CCT therapist ) came down to my level, and so there was never this idea of like, ‘Hey, let’s get you better, come up here with me.’ It was ‘Let’s go down into hell together. Let’s go to the darkest place, and I will be right here with you.’” (Male, 25-44).
Other, more familiar terms were used to describe the CCT therapist, including friend and parent-figure. One participant particularly noted:
“We probably text every couple of days...Every once in a while, I’ll be like, I’m struggling with something - it’s not like I’m struggling 'I want to kill myself.' The CCT therapist always provides very valuable feedback.” (Male 45-64)
Participants also described the CCT therapist in ways that suggested an “outlandish” personality when compared to past therapists:
“I would say that ( CCT therapist ) the demeanor is atypical; I wouldn’t go as far as odd. But I can say the ( CCT Therapist ) demeanor is atypical, but I think it needs to be.” (Female, 45-64).
CCT Program Activities
(Figure 1) shows the typical flow of activities for participants in the CCT program. Many patients were referred to CCT via referrals, and others enrolled in the program after hearing about it from a friend or through a web search for suicide therapy programs. One participant recounts her experience:
Figure 1.Contextual-Conceptual Therapy Program Logic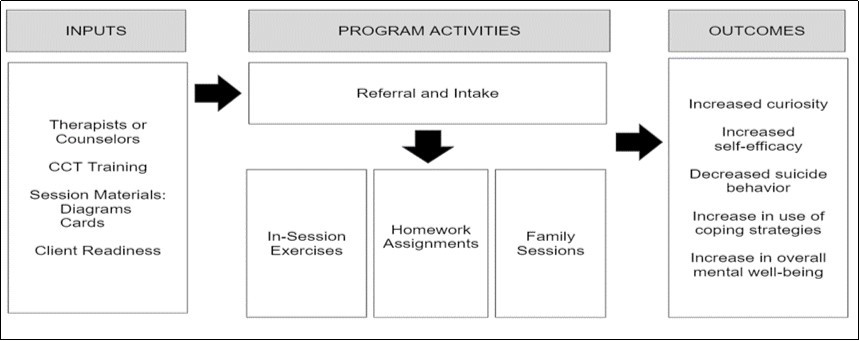
“Through being at that point where I was ready to take my life. . . I called and asked for a referral for doctors in my area. I went and met with her, and she explained to me that she had this person she was in contact with, and it was a little outside of the normal scope of psychiatrist/psychologist that I had seen over the years and wanted to know if I would be willing to indulge in something a little different. And at that point, I was like yes, I am so tired of trying the same over and over again with no results. If you told me to walk backwards on the moon, I would try it ( laughs ) .” (Female 25-44)
The program’s activities aimed to help clients grasp abstract CCT knowledge. Participants noted in 14.9% of codes that the program’s activities were creative (i.e., reading or writing) and allowed them to engage with CCT concepts using their creativity rather than logical thinking. These included in-session exercises, and one participant described a particularly salient exercise:
“The first part was to write, and I uh wrote about something that's meaningful to me, like a movie, or a book, or something, so I wrote about a movie ... And, for part two, I had to cut up just random sentences, and then put those sentences together, um, in my own way onto a construction board...during that process, before I even finished, I found the core…theme throughout my different sentences that I was putting together. And from that opened up ways that I felt about that. It was like something that was behind that I didn't know was there.” (Male, 25-44)
Participants discussed the use of props in the program, such as maps, models, and other figures, and noted that these resonated with them because they helped to illustrate abstract concepts that were otherwise difficult to conceptualize.
“(The client ) was like an emotional Helen Keller when she came in... (The CCT therapist) is a lot like Annie Sullivan because I think [the client) had no symbols, and I think what he did is he gave him symbols, which created a language, which, um, got her out of the dark” (Female, 45-64).
Another Participant Described a CCT Image that she Still Refers to Today
“There’s this graph that (you have) the two “You’s,” and you’re on one side and have your old learning, and on the other side there is a new learning ... in the middle there is just kind of this chasm and it’s called it’s called like ‘depression and disorientation and despair,' and on one part of the graph it talks about suicide and on the other side of the graph, towards the closer side to new learning, it’s enlightenment and new knowledge and that’s how the process is…That graph is something I refer to a lot when I’m going through something hard like, “Okay, this is part of the dissociation process and I know at the end that there will be enlightenment.’” (Female, 25-44).
The homework assignments often kept people busy between their sessions and further assisted in solidifying concepts that they learned in their sessions:
“But after probably two months, I no longer felt like I wanted to kill myself. And I stopped planning how to do it. Uh, and then probably, I was - literally every minute really - was occupied by tasks that (the CCT therapist) assigned me.” (Female, 65+)
“I thought I would just come in and . . . coast my way through the experience, but it became quickly obvious that I was actually selling myself short by doing that.... I found it to be a great recap as well, immediately after, within 24 hours while it was still fresh in the mind … I felt it to be very refreshing, and it solidified the teaching very well, being able to take practice and take part in these exercises really made this an authentic experience.” (Male, 25-44).
Some participants had their family members attend some of the sessions. Many people found these sessions to be helpful, but one participant notes that the timing of initiating family sessions is important to success in the program:
“This was at least six months into the process… So, it’s just hard for someone who hasn’t been a part of a learning process that was so intense, and that kind of intricate, to come in in the middle…if someone’s suicidal, family members are around, then, you know, I guess I would advocate for doing ( family sessions ) sooner rather than later to include everyone.” (Male, 65+)
CCT Program Characteristics
Participants noted that CCT was incomparable to their other therapy. One participant categorized the difference as such:
“Instead of getting narrower, which is what some therapies seem to do you know, trying to find a, a kind of reductionist approach, smaller and smaller to explain bigger and bigger events, um this was just the opposite. It kind of opened the door to explore from any angle that might be pertinent.” (Male, 65+)
One of the defining characteristics that the participants discussed was the programs use of metaphors. One participant described why the use of metaphors is helpful in the program:
“You find any good writer; they write metaphors as a way to cross understanding over to the reader. Metaphors can help people get an understanding.” (Male, 45-64).
The physical office and the CCT therapist’s approach was often described as chaotic, which accounted for 9.6% of codes. Participants noted that the chaos was sometimes frustrating, but most participants acknowledged how this was a necessary characteristic and a key to their success in the program.
“ ( The CCT therapist ) throws a lot at you. A lot of concepts, a lot of ideas...A lot of metaphors, a lot of metaphorical thinking, a lot of different ways of looking at life and it scatters your brain and throws you off balance. It’s the only way you stop seeing things through the template you painted for yourself” ( Male, 45-64).
Participants expressed that the CCT approach dove deep into the root of their problems, and that they felt relief from their mental health symptoms and also felt more complete. Several participants stated that the information and practices that they learned were more sustainable.
“I learn what the core problem is. So, that’s something that can be worked on, instead of trying to change me into something I probably won’t be able to maintain” (Male, 25-44).
Additionally, the knowledge and skills that they learned from the CCT program remained in their arsenal of coping skills even after they concluded regular sessions. One participant stated:
“I think I use skills and concepts daily, hourly, minutely, that I learned from ( the CCT Program ) .” (Female, 25-44)
Barriers accounted for 9.6% of codes. The most common one being the cost to attend the program. One participant stated:
“It’s insane that here’s this thing, this program that can help people so much, but if you can’t afford it, you’ll just then not get the help. Really? ( laughs ) That doesn’t make any sense” (Female, 65+).
Another participant noted the need for a more modern system of delivering the program:
“I found the material that ( the CCT therapist ) uses to be a little antiquated, and he needs a digital revolution in his program. It needs to be like entirely digitalized and gamified because that is an area that I feel would have practical applications across many generations.” (Male, 25-44)
CCT Program Outcomes
Participants experienced a major shift in their mindset, and some participants shared that they felt changes in themselves right away while others noticed a more gradual change. One participant said:
“(After) a month. It wasn’t just like I feel a little better and I’m not suicidal anymore. It’s like the world really looks like a different place. It was almost magical in a strange way. You go from a place where you are so distraught that you are going to kill yourself to like seeing the world completely differently - such a huge change” (Male, 45-64).
One of these changes included feeling more curious about the world, and this accounted for 29.6% of codes, which is quite substantial. In their discussion about curiosity, participants often recited the two rules posed by the CCT therapist: “Don’t believe me, and don’t disbelieve me.” These rules set the foundation for the unique in-session activities that add to the novel, chaotic nature of the program. One participant noted:
“It was always like a new playing field where we could play with stuff and discover stuff together and be curious about stuff and in all of that it helped me figure out how to be different in different ways, that I would’ve never guessed. And as simple as looking at a rock or a picture of someone swimming like just the craziest stuff.” (Male, 25-44)
This increased curiosity begins to manifest even before completion of the program:
“Every week when I would go I would never know what we’re gonna talk about I couldn’t predict it. I couldn’t come up with answers because there wasn’t any, and so there was only the curiosity of what I’m gonna figure out and when I would leave, there would always be kind of, when I would leave that office I would be with so many questions and that would keep me going for another week.” (Male 25-44)
Participants also experienced feelings of empowerment upon completion of the program. Participants felt the ability to find meaning in their lives and confidence that they would make life changes to improve those lives. One participant said:
“(The CCT approach] was like you have everything you need to fix you and I want to help you discover that or find that for yourself… So, I think that was very different and unique. And super important.” (Female, 25-44)
In order to foster their new mindsets, many participants reported drawing, writing, or other creative activities as a means to emote and to exercise the creative side of their mind as part of their new arsenal of coping strategies. One participant described one of his coping strategies as follows:
“Anytime (I’m) outside, if I see something, I carry a little notebook with me, and I write it down. Jot down notes like I see or hear something that’s piqued my interest…later in the day, I would write a story about it.” (Male 25-44)
Discussion
Suicide is one of the ten leading causes of death in the United States and it is without question that recent increases in suicide along with other mental health issues is of serious concern to individuals, communities, practitioners, policy-makers and the country as a whole. Further, much of the suicide prevention research was conducted decades ago, and there is a paucity of newer models and approaches, extending beyond traditional cognitive behavioral therapies. Certainly, suicide has always been a complex and multifaceted public health issue, and given the changing social-ecological landscape of our communities, it is likely that suicide prevention is more complicated than ever. The present qualitative study provided a more systematic examination into an approach that has not yet been evaluated in the literature, Contextual-Conceptual Therapy (CCT). The qualitative results found that (1) CCT is a program that most participants engaged in after a long history of unsuccessful therapies and treatments; (2) CCT is grounded in the destabilization of the logic behind a person’s reasons for suicide and dives deep into root causes; and (3) CCT builds curiosity and self-efficacy which is what yields long term change for its clients. The public health community continues to seek evidence-based solutions for the prevention of suicide, and the findings from this study provide an essential foundation to develop a larger and more robust randomized controlled trial to quantitatively test the efficacy of the CCT approach.
Traditional models that focus on prevention practices as they relate to suicide have often focused on addressing depression and anxiety. And while a person may have thoughts of suicide or attempt suicide as a result of these disorders and illnesses, it may not be the most effective method when preventing suicide ideation and attempt. Through the CCT program, it is clear that changing a person’s curiosity and self-efficacy are incredibly powerful in changing long-term outcomes. The CCT program delves deeper into the root cause of suicide, resulting in a fundamental shift in a person’s mind, and more importantly the person is very aware of that shift occurring.
A recurring theme from the interviews centered around participants’ desires to more widely disseminate the CCT approach, and to find ways in which the program could be replicated at lower costs to the significant numbers of at-risk people in the United States. One participant described how mobile technology and gaming may be a channel of dissemination for CCT. And in fact, taking advantage of the rise in mobile technology, the CCT program could be emulated on a mobile app to help reach millions of individuals not only in the U.S. but globally.
Training therapists to implement the CCT approach is a significant investment of time and resources. Therefore, future studies should explore how to scale the training of health professionals to broaden the program’s reach. Anecdotal evidence from CCT associates and therapists indicate that the trainings are quite successful and new CCT associates are able to pick up this new approach quickly. As the CCT approach expands, it will be important to ensure that materials are fully standardized, and that there are booster trainings and other types of support for CCT therapists in order to maintain the quality and the fidelity of the program.
Further, while the CCT program is suicide-specific, many of the program components are salient to broader mental health concerns. Future studies should explore how specific program components can be adapted to address other mental health issues and illnesses, as well as to foster mental well-being among a diverse population of children and adults.
And finally, although these findings compel an urgency to further evaluate the efficacy of CCT and potential derivates of the CCT approach, this study had several limitations. First, these are cross-sectional qualitative data and therefore lends itself to hypothesis generation and does not imply causal inferences. Second, the study focused on a small sample of recent CCT clients and may not be fully generalizable. Despite these limitations, this study provides important insights for wider dissemination of the program and a future efficacy trial.
Conclusions
At a time when a diverse mental health is impacting the lives of millions, the CCT program has the potential to help individuals change their mindsets, moving away from their deep feelings of hopefulness and despair. The results of this qualitative analysis are an important first step in understanding effective suicide prevention programs. However, to fully assess the impact of the program, a randomized control trial should be conducted to measure short and long term outcomes among diverse populations, and to better understand how to meet the needs of mental well-being in all populations.
Ethics
All procedures for this study, including protection of human subjects, were reviewed and approved by the Institutional Review Board (IRB) at the GW Office of Human Research (IRB#NCR191356)).
Acknowledgements
This manuscript and study are a product of a highly collaborative team. We would like to thank Fredric Matteson, the founder of the CCT approach for his dedication to healing and his thoughtful and creative approach to suicide prevention. We would also like to thank Elliott Donnelly for his support and insights about the program and its public health impact. We are indebted to our research interns who assisted with transcribing and coding interviews. And we are incredibly grateful to the study participants who generously and graciously offered us their time, reflection, honesty, and authenticity.
References
- 1.Stack S. (2000) Suicide: A 15-Year Review of the Sociological Literature. Part I: Cultural and Economic Factors. Suicide and Life-Threatening Behavior. 30(2), 145-162.
- 2.National Institute of Mental Health. Mental Health Information. Statistics. Suicide. Available at: https://www.nimh.nih.gov/health/statistics/suicide.shtml
- 3. (1999) The Centers for Disease Control and Prevention. (CDC). Suicide Mortality Rates in the U.S Available at: https://www.cdc.gov/nchs/products/databriefs/db330.htm .
- 4.The Centers for Disease Control and Prevention. CDC Newsroom. Death Rates up for 5 of the 12 Leading Causes of Death. Available. at: https://www.cdc.gov/media/releases/2018/p0920-death-rates-up.html
- 5.The Centers for Disease Control and Prevention. Vital Signs. Suicide Rates Across the U.S. Available at: https://www.cdc.gov/vitalsigns/suicide/index.html.
- 6.The Centers for Disease Control and Prevention. Injury. Injuries Cost the U.S. $671 Billion in the U.S. Available at: https://www.cdc.gov/injury/pdfs/wisqars/cost-slides-2015-a.pdf .
- 7.D M Stone, K M Holland, Bartholow B, A E Crosby, Davis S et al. (2017) Preventing Suicide: A Technical Package of Policies, Programs, and Practices. Atlanta,GA: National Center for Injury Prevention and Control,Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/violenceprevention/pdf/suicideTechnicalPackage.pdf.
- 8.S U. (2012) Department of Health and Human Services (HHS) Office of the Surgeon General and National Action Alliance for Suicide Prevention. , Washington, D.C:
- 9.Asarnow J, Hughes J, Babeva K, Sugar C. (2017) Cognitive-Behavioral Family Treatment for Suicide Attempt Prevention: A Randomized Controlled Trial. , Journal of theAmerican Academy of Child & Adolescent Psychiatry 56(6), 506-514.
- 10.American Foundation for Suicide Prevention. Suicide Statistics. Available at: https://afsp.org/about-suicide/suicide-statistics/.
- 11. (2018) Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the. National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068 NSDUH Series H-53). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Available at: https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHFFR2017/NSDUHFFR2017.pdf .
- 12.Zalsman G, Hawton K, Wasserman D, K van Heeringen, Arensman E et al. (2016) Suicide prevention strategies revisited: 10-year systematic review. , TheLancet Psychiatry 3(7), 646-659.
- 13.R C Kessler, Berglund P, Demler O, Jin R, K R Merikangas et al. (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. , Arch Gen Psychiatry 62(6), 593-602.
- 14.C S Harrod, C W Goss, Stallones L, DiGuiseppi C. (2014) Interventions for primary prevention of suicide in university and other post-secondary educational settings. Cochrane Database Syst Rev,10.
- 15.Cusimano, Sameem M. (2011) The effectiveness of middle and high school-based suicide prevention programmes for adolescents: a systematic review. , InjPrev 17, 43-49.
- 16.Katz C, S L Bolton, L Y Katz, Isaak C, Tilston-Jones T et al. (2013) A systematic review of school-based suicide prevention programs. , Depress Anxiety 30, 030-1045.
- 17.Klimes-Dougan B, D A Klingbeil, S J Meller. (2013) The impact of universal suicide-prevention programs on the help-seeking attitudes and behaviors of youths. , Crisis 34, 82-97.
- 18.Robinson J, Cox G, Malone A. (2013) A systematic review of school-based interventions aimed at preventing, treating, and responding to suicide-related behavior in young people. , Crisis 34, 164-182.
- 19.Ciffone J. (2007) Suicide Prevention: An analysis and replication of a curriculum-based high school program. , Soc Work 52, 41-49.
- 20.Freedenthal S. (2010) Adolescent help-seeking and the yellow ribbon suicide prevention program: an evaluation. , Suicide Life Threat Behav 40, 628-639.
- 21.Hooven C, J R Herting, K A Snedker. (2010) Long-term outcomes for the promoting CARE suicide prevention program. , Am J Health Behav 34, 721-736.
- 22.National Institute of Mental Health. (n.d.). Suicide Prevention. Web. Available at: https://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml
- 23.O’Connor E, B N Gaynes, B U, Soh C, E P Whitlock. (2013) Screening for and treatment of suicide risk relevant to primary care: a systematic review for the U.S. Preventive Services Task Force. , Ann Intern Med 158, 741-758.
- 24.Hofmann S, Asnaani A, Vonk I, Sawyer A, Fang A. (2012) The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. , Cognitive Therapy and Research 36(5), 427-440.
- 25.Chapman A. (2006) Dialectical behavior therapy: current indications and unique elements. , Psychiatry (Edgmont (Pa Township)) 3(9), 62-68.
