Massive Splenic Rupture – An Unusual Presentation
Abstract
A case report of massive splenic rupture with atypical presentation. It covers diagnostic work‑up, stabilization, and operative decision‑making.
Author Contributions
Academic Editor: Junfei Jin, Laboratory of Hepatobiliary and Pancreatic Surgery, Affiliated Hospital of Guilin Medical University (China)
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2016 Shiva Seetahal, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Case
A 61 year old Caucasian male, visiting from the UK, presented to the Emergency Room (ER) complaining of a chronic cough for 2 weeks and new-onset dizziness. The cough was non-productive but recalcitrant to antitussives. His dizziness was exacerbated with exertion and associated with palpitations and sweating. While in the ER, he also started experiencing generalized abdominal pain. His medical history included hypothyroidism and hypertension, both adequately controlled with medications. His annual physical and blood work, done 3 months prior in the UK, was unremarkable by his account.
Vitals signs included an initial blood pressure of 109/58 mmHg and sinus tachycardia. Physical exam revealed an asymmetrically distended abdomen with rebound tenderness and splenomegaly, and decreased breath sounds in the left lung base. Hemoglobin on admission was 10.9 g/dl which dropped to 9.1 g/dl; his white blood cell count (WBC) was 139 (x 109 /L). Although the patient and his wife were visiting the area to indulge in the local theme parks, he denied participating in any of the rides owing to malaise from his cough. He also denied any trauma to the torso area in recent times.
A plain abdominopelvic CT showed massive splenomegaly with high attenuation areas suspicious for hematoma, as well as free fluid in the abdomen (Figure 1). The patient was immediately started on a transfusion of packed red blood cells and taken emergently to the operating room. A laparotomy was performed and the patient was found to have a massive, ruptured spleen with 1500 mls of frank blood in the peritoneal cavity. Splenectomy and abdominal washout were done. The spleen measured 21 x 19 x 10 cm and weighed 2870 grams. It is shown below (Figure 2).
Figure 1.CT image of the abdomen showing the enlarged spleen. The arrows point to areas of higher attenuation suspicious for hematoma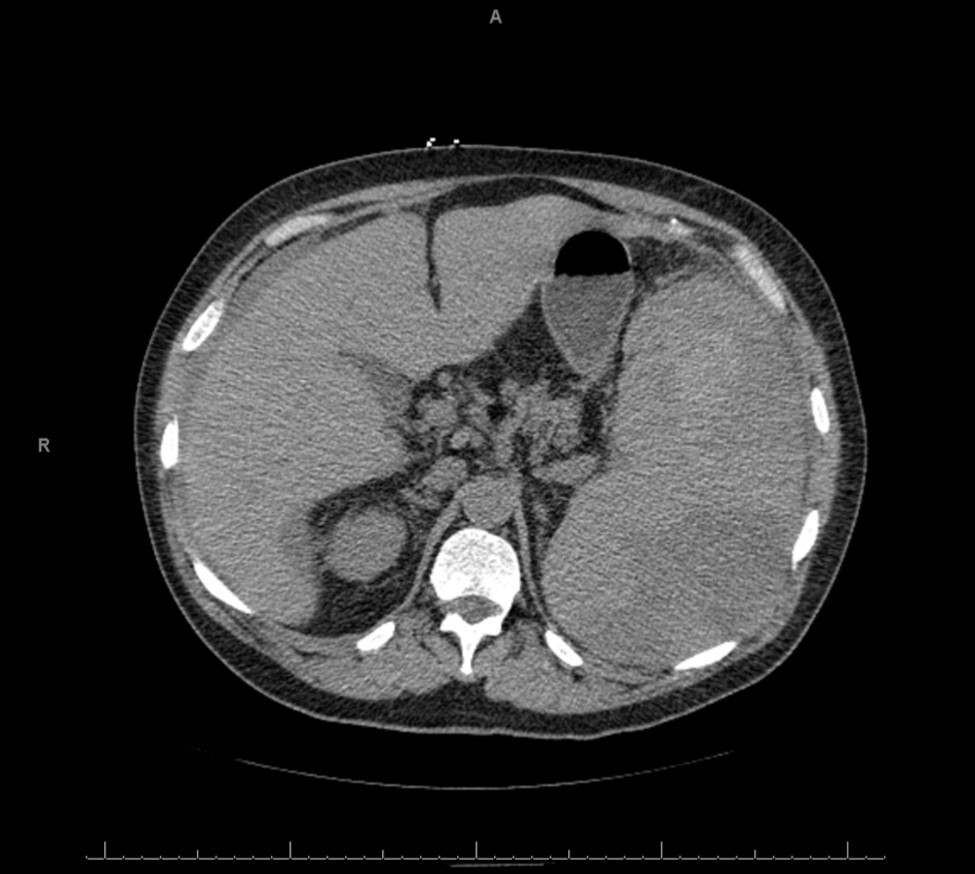
Figure 2.Spleen following removal – medial and hilar aspect shown. Arrow points to area of rupture.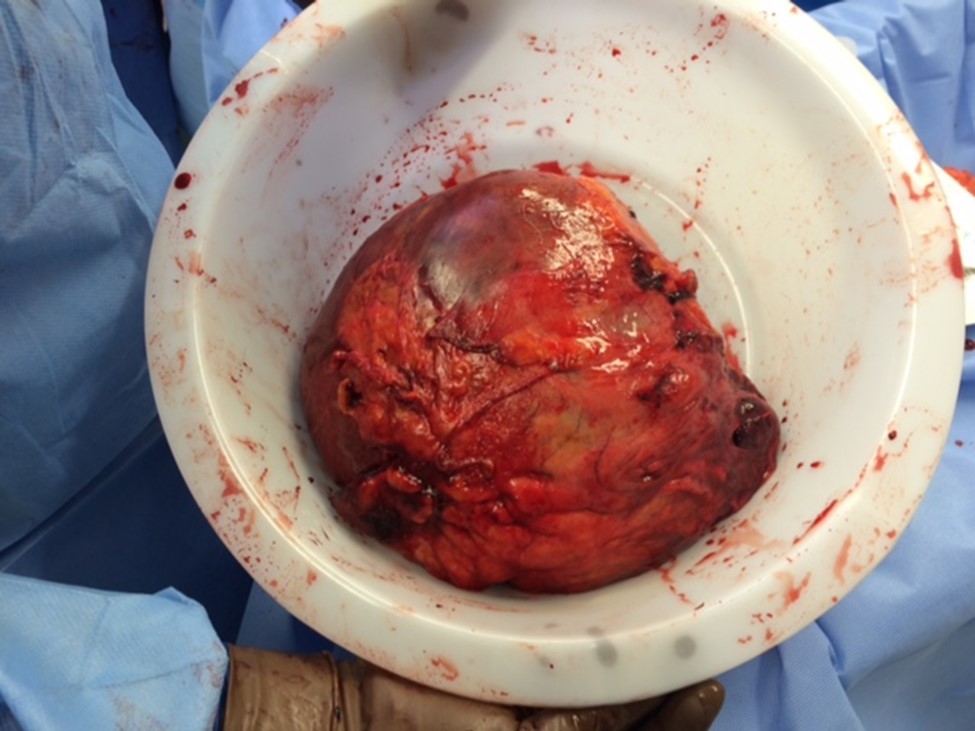
1. Postoperatively, the patient recovered well and was discharged 4 days later. Pathology of the spleen showed a predominance of maturing myeloid cells and was consistent with chronic myelomoncytic leukemia (CML).
Discussion
CML is disorder of the bone marrow`s stem cells that results in a proliferation of granulocytes in various stages of maturity. The incidence is roughly 1.5 in 100,000 and accounts for 10-15% of all leukemia types. It is more common in males and has a median age of diagnosis of 65 years, being extremely rare in children. It is associated with the chromosomal translocation best known as the Philadelphia (Ph) chromosome. The Ph chromosome was discovered in 1960. It represents a translocation of genetic material between chromosomes 22 and 9 to create a fusion gene BCR-ABL1. This gene leads to permanent activation of a specific transmembrane tyrosine kinase receptor located on myeloid precursor cells in the bone marrow. These cells proliferate at an uncontrolled rate and eventually overwhelm the bone marrow and spread to infiltrate other organs such as the spleen and liver 1. Splenomegaly is a common feature owing to the massive proliferation of granulocytes that infiltrate the organ. The degree of splenomegaly can be correlated with the granulocyte count of the peripheral blood and massive spleens can be a precursor to an acute blast crisis 2. However, spontaneous splenic rupture is unusual.
Various theories have been proposed as to the mechanism behind spontaneous splenic rupture in hematological disorders. The most widely held is that the direct infiltration of the organ with massive amounts of malignant cells eventually overwhelms its ability to compensate and expand, leading to breaches of the capsule. This manifests as progressive splenomegaly, often asymptomatic until discovered incidentally or as a consequence of capsular breach and hemorrhage. Another theory describes the rapid expansion of the organ causing disruption of the blood supply and areas of infarction that are more susceptible to breakdown. This theory would be more germane to patients who suffer blast crises, as these events lead to rapid and profound splenic engorgement 3, 4, 5.
In patients with massive splenomegaly (spleen diameter > 20cm), the risk of traumatic rupture is considerable. The spleen is normally protected below the left lower ribs, but as it enlarges, the inferior and medial aspects expand beyond those borders are become susceptible to injury. The patient in this case was lucky to have avoided the rougher rides and roller-coasters that would have placed him at risk for potentially catastrophic splenic injury. There are case reports of blunt splenic trauma from such rides 6. That same luck unfortunately did not prevent him from presenting with a rare complication of his underlying condition.
Treatment of splenic rupture is dependent on the hemodynamic stability of the patient at the time of presentation. If the patient is hemodynamically stable and the appropriate facilities are available, angiography and splenic artery embolization can be attempted. The success rates for angioembolization are improving over the last decade; this is now the preferred initial management for the majority of splenic injuries. Interventional radiology staff and equipment, as well as an adequate supply of blood products are essential to the success of this approach 7, 8. In the unstable patient, expeditious exploration is warranted. Midline laparotomy approaches provide expeditious exposure; left subcostal incisions are an alternate route. In patients in hemorrhagic shock, laparoscopic exploration is inappropriate. Splenoraphy or partial splenectomy are options only if the patient`s condition can be stabilized, otherwise complete splenectomy is definitive. The organ should be mobilized from its lateral and superior attachments to allow it to be rotated anteromedially. This facilitates rapid vascular control and arrest of the bleeding. Once vascular control has been achieved, a decision can be made regarding the possibility of splenic preservation 9, 10. Current guidelines advocate splenic preservation when possible owing to concerns about post-splenectomy infections. The patient in this case had such massive splenomegaly and severe blood loss, that complete splenectomy was necessitated.
References
- 1.Kurzrock R, Kantarjian H M, Drucker B J, Talpaz M. (2003) Philadelphia chromosome positive leukemias: From basic mechansims to molecular theories. Ann Intern Med. 138(10), 819-30.
- 2.Karkuzhali P, Shanthi V, Usha T. (2013) A case of chronic myeloid leukemia presenting as megakaryocytic blast crisis (AML M7). Ecancermedicalscience. 21, 375.
- 3.Bauer T W, Haskins G E, Armitage J O. (1981) Splenic rupture in patients with hematologic malignancies. Cancer. 48, 2729-33.
- 4.Jafferbhoy S, Chantry A, Atkey N, Turner D, Wyld L. (2011) Spontaneous splenic rupture: an unusual presentation of CML. BMJ Case Rep.
- 8.Brillantino A, Iacobellis F, Robustelli U, Villamaina E, Maglione F. (2015) Eur J Trauma Emerg Surg.
