Pseudotumor Tuberculosis Of Liver: A Rare Entity
Abstract
We present a rare case of a 46-year-old man who presented with recurrent fever and abdominal pain without other symptoms. Laboratory data were no specific for diagnosis. Abdominal imaging revealed a pseudotumor liver. A diagnosis of isolated liver tuberculosis with abscess component was confirmed with US-guided liver biopsy and histopathological examination. The patient received antibacillous drugs with success.
Author Contributions
Academic Editor: Junfei Jin, Laboratory of Hepatobiliary and Pancreatic Surgery, Affiliated Hospital of Guilin Medical University (China)
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2015 Mehdi Soufi, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation:
Introduction:
Tuberculosis is one of the most common diseases in Morocco 1. Although the prevalence of tuberculosis decreased quickly worldwide after the widespread use of antibacillous drugs, the prevalence has increased in recent years in immunocompromised and immunocompetent patients 1. Hepatic tuberculosis is an uncommon form of extrapulmonary tuberculosis. It is usually a disseminated disease associated with military tuberculosis, which is one of the most characteristic manifestations of tuberculosis. Localized tuberculosis of the liver in the pseudotumor form is rare 2. We report a rare case of isolated liver tuberculosis in young patient without any immunodeficiency treated successfully with antibacillous drugs.
Case Report:
A 46 year old man was admitted with 5 months history of remittent fever ranging between 37.6°C and 38.2°C. The fever was associated with chills and epigastric pain, as well as night sweats. The patient has also a history of 10 Kg weight loss along with loss of appetite. On clinical examination, the patient was, oriented in time and space, cooperative, febrile 37,9, anicteric and normopneic, without peripheral lymphadenopathy. He had abdominal tenderness in the epigastric region, without hepatosplenomegaly.
Laboratory analysis showed hemoglobin, 10.9 g/dL; white blood cell count, 9,800 cells/mm3, serum albumin, serum total bilirubin, alanine aminotransferase, aspartate aminotransferase, prothrombin time, hepatitis B surface antigen, and antibodies to hepatitis C, serum alpha-fetoprotein (AFP), carcinoembryonic antigen and carbohydrate antigen 19-9 (CA 19-9) were within normal range. Blood cultures were negative. Chest x-ray was normal. Ultrasound of abdomen showed a 10 cm hypoechogenic lesion in left liver (Figure 1). An abdominal CT showed a well-defined heterogeneous mass situated in his left hepatic lobe measuring 10 cm × 7 cm (Figure 2, Figure 3). The lesion featured central necrosis, a hyper-dense rim and a mild enrichment from the arterial phase in the CT, The diagnosis of primary hepatic tumor was suspected. An ultrasonography-guided needle biopsy of the liver was scheduled in order to rule out malignancy and to have a complete diagnosis. Cytology demonstrated a tuberculosis granuloma, acid-fast bacilli culture was positive (Figure 4). Anti-tuberculous therapy including isoniazid, rifampin, ethambutol, and pyrazinamide were prescribed. The patient completed the 6-month course of medication with success. The patient’s appetite and body weight were restored to previous levels. One year after the completion of treatment, the patient remained completely asymptomatic with disease free.
Figure 1.Ultrasonography showing a 10 cm hypoechoic lesion
Figure 2.Abdominal computed tomography with intravenous contrast showing 10x7 cm low-density focal lesion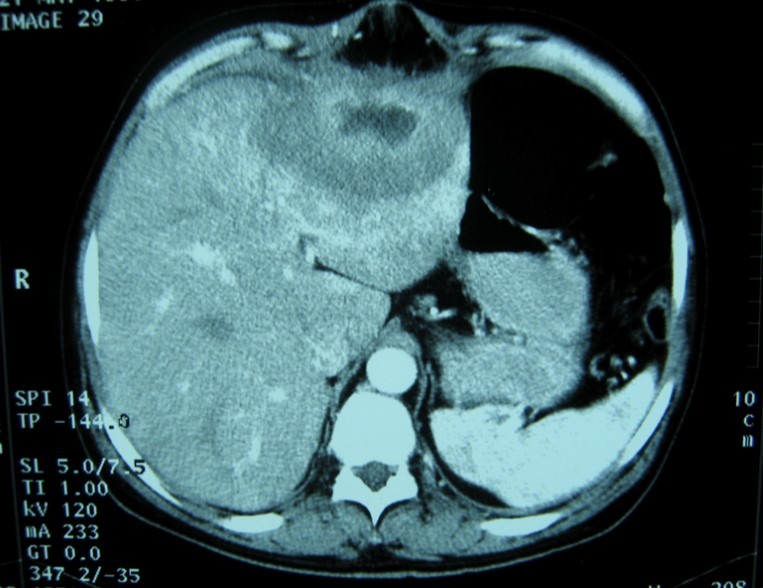
Figure 3.Abdominal computed tomography with intravenous contrast showing the lesion with ring enhancement.
Figure 4.Hepatic histopathology of patient showing granuloma
Discussion
Tuberculosis is a health problem in the developing countries 1. It remains a healthcare challenge in the developed world probably due to increased immigration as well as to an increase in patients with the acquired immunodeficiency syndrome (AIDS) 2. Since 1950, 21 cases of isolated tuberculoma or tuberculous abscess of the liver have been reported in the world literature. Abdominal tuberculosis is a rare manifestation of extrapulmonary forms. Hepatobiliary tuberculosis is rare 3. Usually it is associated with foci of infection in the lungs or gastrointestinal tract 4.
Diffuse hepatic involvement with pulmonary or miliary tuberculosis is the most frequent forms in hepatic tuberculosis. The second common form is granulomatous hepatitis. It is a diffuse hepatic infiltration without pulmonary involvement. In our patient the lesion was a pseudotumor of the liver and presents the third form as a focal local tuberculoma or abscess 5.
Tuberculosis spreads to the liver through the hepatic artery, the portal system and the lymphatic system. It commonly involves the hepatic parenchyma and sometimes the biliary tree 4, 6. Both caseating and non-caseating granulomas were described. Focal tuberculosis appears as nodules with calcifications. These nodules are sometimes the source of hematogenic spread 6, 7. The diagnosis can be easy if all criteria established by Maharaj et al are found such as hepatic granuloma with or without Langhans-type giant cells, and/or caseation plus tubercle bacilli elsewhere 8. A previous history of tuberculosis infection should help for the diagnosis. Pseudotumor liver is an uncommon manifestation of hepatic tuberculosis. The clinical presentation is not specific and a high degree of clinical suspicion is required to diagnose the entity 9. The most common symptoms are right upper quadrant pain, fever, anorexia, and weight loss. The clinical features of local form hepatic tuberculosis are variable. Hepatomegaly and splenomegaly are common and liver is often tender and nodular 4, 9. Although liver function tests were normal in our case, abnormal Liver Function Tests may be present. Anemia and elevated erythrocyte sedimentation rate are often seen 10.
Imaging is useful for diagnosis. Abnormal chest x-rays demonstrating pulmonary tuberculosis can help for diagnosis. Our patient presented with no evidence of active pulmonary disease and the ultrasonography showed a hypoechoic rim and solitary lesion. In theses cases, it is difficult to differentiate them from carcinoma 11.
Computed tomography (CT) and magnetic resonance imaging (MRI) are helpful in diagnosis.
CT findings of tuberculosis abscesses can show low-density focal lesions with or without ring enhancement on contrast administration. These have also been seen in necrotic tumor such as hepatocellular, inflammatory disease and metastatic carcinoma 12.
CT-guided aspiration and biopsy can confirm the diagnosis. Percutaneous needle biopsy of the liver using ultrasound, CT has greater than 90 percent sensitivity. In case of pseudotumor tuberculosis mimicking a carcinoma, the role of biopsy is important because it can change therapeutic attitudes. The definitive diagnosis of this disease is conventionally made by histological analysis of caseating granuloma or demonstration of acid-fast bacilli on culture of biopsy specimen 13.
Otherwise, the rate of accurate pretreatment diagnosis by guided percutaneous liver biopsy has been reported to be low, and the presence of tubercle bacilli in the biopsy sample is rare. In these cases, using polymerase chain reaction to directly detect the presence of Mycobacterium tuberculosis improves sensitivity rates 14.
CT drainage is good for the successful drainage of tubercular abscess, although surgical drainage may occasionally be required 15.
The treatment of hepatobiliary tuberculosis does not differ from other extrapulmonary tuberculosis. We usually use Chemotherapy with standard anti-tuberculosis drugs. This is true for both diffuse as well as the local forms of the disease. In general, a 6- to 9-month regimen (2 months of Isoniazid, Rifampin, Pyrazinamide, and Ethambutol followed by 4–7 months of isoniazid and rifampin) is the recommended treatment for extrapulmonary tuberculosis 3, 10, 16.
The surgical treatment is most often indicated when a diagnosis of liver tumor is assumed. In these cases therapeutic modalities include all kinds of hepatic resection with postoperative administration of antituberculous agents 17.
The prognosis remains excellent with appropriate antibacillous treatment. The Mortality rate for hepatic tuberculosis is higher in immunodeficient patient. Predictive factors of mortality are age under 20 years, miliary tuberculosis, concurrent steroid therapy, AIDS, cachexia, associated cirrhosis and liver failure 10.
Conclusion
Liver tuberculosis is a rare and curable disease. The clinical presentation of isolated liver tuberculosis is non-specific. Preoperative diagnosis when it presents, as pseudotumor lesions are difficult. Histopathology is necessary for diagnosis. Because of the increasing incidence of tuberculosis, clinicians should be aware of the possibility of tuberculosis disease with liver pseudotumor.
Competing Interest:
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Kizub D, Ghali I, Sabouni R, Bourkadi J E, Bennani K et al.(2012)Qualitative study of perceived causes of tuberculosis treatment default among health care workers in Morocco. , Int J Tuberc Lung 16(9), 1214-20.
- 2.Bernabeu Mora R, Paredes Reyes P, Latour Pérez J, Méndez Martínez P, Lorenzo Cruz M et al. (2002) Tuberculous liver abscess in an immigrant patient with pulmonary tuberculosis . , Arch Bronconeumol 38(5), 246-8.
- 3.Soufi M, Benamer S, Chad B. (2011) Pseudotumoral gallbladder tuberculosis. , Rev Med Interne 32(3), 32-3.
- 4.Gallinger S, Strasber S M, Marcus.HI(1986). Local hepatic tuberculosis, the cause of a painful hepatic mass: case report and review of the literature. , Can J Surg 29, 451-2.
- 6.Richard R Rau, Lynn C Ricketts.. Bevans .( 1976) Tuberculous pseudotumors of the liver .Am j med 61(6), 946-951.
- 7.Sonika U, Kar P. (2012) Tuberculosis and liver disease: management issues. Trop Gastroenterol. 33(2), 102-6.
- 8.Maharaj B, W P Leary, D J Pudifin. (1987) A prospective study of hepatic tuberculosis in 41 black patients. , Q J Med 63, 517-22.
- 9.Lee S W, Lien H C, Chang C S. (2010) Tuberculous liver abscess in a case without lung involvement. , Kaohsiung J Med Sci 26(2), 99-104.
- 11.Cao B S, Li X L, Li N, Wang Z Y. (2010) The nodular form of hepatic tuberculosis: contrast-enhanced ultrasonographic findings with pathologic correlation. , J Ultrasound Med 29(6), 881-8.
- 12.Yu R S, Zhang S Z, Wu J J, Li R F.(2004).Imaging diagnosis of 12 patients with hepatic tuberculosis.World. , J Gastroenterol 10(11), 1639-42.
- 13.Lee W K, F Van Tonder, Tartaglia C J, Dagia C, Cazzato R L et al. (2012) CT appearances of abdominal tuberculosis. , Clin Radiol 67(6), 596-604.
- 14.Alcantara-Payawal D E, Matsumura M, Shiratori Y, Okudaira T, Gonzalez R et al. (1997) Direct detection of Mycobacterium tuberculosis using polymerase chain reaction assay among patients with hepatic granuloma. , J Hepatol 27(4), 620-7.
- 15.Wilde C C, Kuch Y K. (1991) Case report : Tuberculous hepatic and spleenic abscess. , Clin Radiol 43, 215-6.
Cited by (1)
This article has been cited by 1 scholarly work according to:
Citing Articles:
Journal of Spleen and Liver Research (2015) OpenAlex
