A Newer Approach in the Management of Cough: A Review on Levodropropizine
Abstract
Safe and effective antitussive therapy remains a significant area of unmet need for cough management. Antitussive drugs are commonly used cough suppressants and include centrally acting (opioids and non-opioids) cough suppressants and peripherally acting antitussives. Authors searched PubMed, Google Scholar and additional studies from reference lists via cross-referencing to identify studies assessing levodropropizine for the treatment of cough. Of the 748 studies identified, 13 were included. Recent clinical evidence, guideline recommendations and findings from this review suggest that levodropropizine is a peripheral antitussive which reduces cough intensity, frequency, and nocturnal awakenings in children and adults and provides better efficacy outcomes with a more favourable risk/benefit ratio compared to centrally acting antitussive agents which pose greater safety concerns and present an unacceptable risk–benefit profile. This review is aimed at Indian primary care physicians for making effective cough management decisions where the clinical evidence needs to be translated to clinical practice.
Key Messages
The usage of currently available centrally acting antitussive agent is greatly limited by their central depressing action and frequent side effect. The findings of this review indicate that levodropropizine is an effective antitussive agent and well tolerated in the management of cough in patients of all ages.
Author Contributions
Academic Editor: Sasho Stoleski, Institute of Occupational Health of R. Macedonia, WHO CC and Ga2len CC
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2023 Thomas Prasanna K, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
Dr. Prasanna K Thomas, Dr. Pramod Jog, Dr. Nitin R Vohra, have no competing interests. Dr. Krishna C Veligandla and Dr. Anup U Petare are Dr. Reddy's Laboratories Ltd employees.
Citation:
Introduction
Coughing is a vital defensive reflex that allows clearance of excessive airway secretions and prevents the entry of foreign bodies into the respiratory tract. 1 Cough is classified into three categories based on its duration: acute (<3 weeks), subacute (3-8 weeks), and chronic (>8 weeks in adults and >4 weeks in children). 2, 3, 4 Acute cough episodes are mainly related to upper respiratory tract infections (URTI). The other underlying causes of acute cough are pneumonia, congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD) exacerbation, aspiration, and pulmonary embolism. 5
The American College of Chest Physicians (ACCP) defines subacute cough as cough that resolves spontaneously on its own, with negative chest radiography ruling out pneumonia4 Chronic cough can be caused by many diseases including asthma, gastroesophageal reflux disease (GERD), chronic bronchitis, bronchiectasis, and postnasal drip.6 Cough can also be categorized based on the sputum volume as dry and wet cough. Wet cough is also known as productive cough and is defined as sputum volume >10 mL per day.4,7 A dry cough is also known as unproductive cough and is characterized by no mucus production. Chronic cough may indicate a more serious underlying medical condition such as asthma, postnasal drip, and gastric reflux disease.8 Patients with the acute and sub-acute cough usually self-medicate with over the counter (OTC) antitussive drugs, although a careful examination and patient history is required to identify the underlying causes. OTC drugs which include combinations of antihistamines, decongestants, cough suppressants and expectorants are most used preparations for self-medication.9 Current ACCP guidelines recommend nonpharmacologic and pharmacologic treatments based on patient comorbid disease status and underlying chronic cough causes. Pharmacologic treatment usually consists of a bronchodilator, corticosteroid, leukotriene receptor antagonists and inhaled anticholinergic etc. 10 Antitussive drugs are commonly used cough suppressants which include centrally acting (opioids and non-opioids) cough suppressants and peripheral antitussives. Codeine, dextromethorphan and cloperastine are among the most common central agents that act by inhibiting the cough center in the brain.11 Peripherally acting antitussives such as levodropropizine and moguisteine exhibit a very strong antitussive activity. Levodropropizine is an orally administered non-opioid anti-tussive agent whose peripheral antitussive action may result from its modulation of sensory neuropeptide levels within the respiratory tract.12, 13, 14 In India, levodropropizine was approved by The Central Drugs Standard Control Organization in 2005 for the treatment of dry cough in adult patient. 15 The current ACCP and ERS guidelines also suggest using alternative antitussive strategy in subset of patients with cough resistant to other treatments.16
There is a need to find an effective antitussive medication with a high tolerability profile because the usage of the currently available centrally acting antitussive for the treatment of cough is severely restricted by the central depressive action and abusive side effects. 17 This review article aims to summarize the potential mechanism of action, comparative effectiveness, and safety profile of levodropropizine for symptomatic treatment of cough in paediatric and adult population. Its impact on patients’ health-related quality of life (HRQoL) and in managing COVID-19 associated cough have also been discussed.
Methods
Data sources and searches
A comprehensive literature search was carried out on the PubMed databases to identify clinical studies and meta-analyses of levodropropizine for the treatment of cough in the adult or paediatric population. The search terms were ((cough) OR (chronic cough) OR (acute cough)) AND ((levodropropizine) OR (peripheral antitussives) OR (central antitussives) OR (codeine) OR (dihydrocodeine) OR (dextromethorphan) OR (dropropizine)) for articles published in peer-reviewed journals from their inception through November 2022. Additional searches were conducted in Google Scholar and from review article reference list through cross-referenced articles. There were no language restrictions. The search was restricted to studies conducted in human populations.
Study selection criteria
Following are the inclusion criteria used to select studies: Clinical studies (vs. both active-and placebo-controlled) and meta-analysis design, including paediatric and adult patients, and assessing efficacy endpoints related to cough outcomes, safety results, or quality of life data were selected. Patients of any age suffering from cough types such as chronic cough, lung cancer cough, moderate non-productive cough, bronchitis cough, acute cough caused by URTI, non-productive cough, or asthmatic cough were included in the narrative review. Studies using duplicate samples, case reports, editorial, letter were excluded. In determining eligibility, discrepancies were resolved through consensus among authors. Of the 748 studies identified, 13 were included. Out of 13 included studies, nine published clinical studies were conducted with levodropropizine in adults or children and met the eligibility criteria for efficacy and safety data, two studies were included for the impact on patients’ HRQoL, and one for the role of levodropropizine in the management of COVID-19-related cough and one meta-analysis that evaluated the pooled estimates of efficacy in adults and children were selected for summarizing the published evidence.
Data extraction
For all the included articles for comparative efficacy and safety parameters, we extracted and confirmed the data. The extracted outcomes included study design, sample size, participant age, comparator, indication or condition, dosing schedule, efficacy result and safety result.
Mechanism of action
Levodropropizine is a peripherally acting non-opioid antitussive agent that acts by inhibiting sensory neuropeptide release in the respiratory tract and suppresses the pulmonary afferent pathway. 18 Levodropropizine (S(-)3-(4-phenyl-piperazin-1-yl)-propane-1,2-diol, DF 526) is the l-isomer of dropropizine, which is a racemic drug widely used in cough management. Compared with its racemate, levodropropizinehad weaker central sedative effects. It exerts cough suppressant effect through an inhibitory action of the airway sensory nerves with modulation of sensory neuropeptides within the respiratory tract. Levodropropizine also leads to in vitro inhibition of neuropeptides release from C-fibers. Levodropropizine exerts its cough suppressant effect by acting on H1-histaminic and alpha-adrenergic receptors. 11, 18, 19 The peripheral mode of action of levodropropizine provides better efficacy outcome with a more favourable risk/benefit ratio when compared with centrally active drugs such as dextromethorphan. 11, 18
Pharmacokinetics
Levodropropizine has linear pharmacokinetic (PK) characteristics at doses ranging from 30 to 90 mg. After oral administration, levodropropizine is rapidly absorbed into the intestine and goes into first pass metabolism, with reaching its maximum drug plasma concentration (Cmax) within 0.25 to 0.75 hours (Tmax). 19,20 Levodropropizine faster onset of action is due to high bioavailability (75%) and rapid distribution in the body compartment. The mean terminal half- life (t1/2) of levodropropizine is 2.73 h, which resulted into rapid elimination after systemic absorption. 14,20,21 The faster onset of action and high bioavailability of levodropropizine ensure rapid relief from cough in comparison with centrally acting anti-tussive. 14, 21
Comparative efficacy of levodropropizine
Levodropropizine is an effective antitussive drug in patients of all ages that has shown statistically significant better outcomes compared with central antitussive agents in terms of efficacy, tolerability, reducing cough intensity, frequency, and night awakenings. 11 Levodropropizine has also been shown to be significantly better in overall efficacy outcomes in cough suppressant caused by various underlying diseases, including dry cough in patients with lung cancer, tuberculosis and URTI.3
Evidence from randomized controlled trials
Adults
Table 1shows the studies conducted in adults. In a double blind, double dummy two parallel groups, randomized study carried out by Allegra et al., the efficacy of levodropropizine was compared to the placebo, and two central antitussive drugs, i.e., morclofone and cloperastine. The antitussive activity and therapeutic efficacy of levodropropizine in this study was higher than placebo as well as morclofone, whereas it was comparable to cloperastine. About 80% of patients responded to levodropropizine and cough frequency was reduced in 33-51% of patient. 22 The efficacy of levodropropizine vs. dextromethorphan in oral dose for 5 days on moderate non-productive cough was investigated by Catena et al. in a small double blind randomized study in 209 adult patients. Both antitussives significantly decreased cough frequency over the course of treatment, but levodropropizine onset of action and effect was faster than dextromethorphan. Levodropropizine significantly reduced the number of night awakenings and improved cough relief after the second day of treatment than dextromethorphan. 23 Another double-blind randomized study was conducted by Luporini et al. to evaluate the efficacy of levodropropizine as compared to central antitussive drug dihydrocodeine. The results obtained in this trial confirmed the superior benefit/risk profile of levodropropizine than dihydrocodeine (Table 1). 24
Table 1. Comparative efficacy of levodropropizine vs control| Study | Study design | Sample size | Participant age (Year) | Comparator | Condition | Dosing schedule | Efficacy results | Safety result |
|---|---|---|---|---|---|---|---|---|
| In adult patient | ||||||||
| Lee 2022 30 | Open-label, RCT | 88 | 50.83 | Codeine | Chronic cough | Orally administered codeine (60 mg/day) and LDP (180 mg/day) for two weeks | Codeine & LDP are effective antitussive for chronic cough | Frequency of TEAEs was substantially higher in the codeine group than in the LDP group (44.4% vs. 14.0%, P = 0.002) |
| Luporini 1998 24 | RCT (double-blind) | 140 | > 18 | Dihydrocodeine (DHC) | Lung cancer cough | Oral administration t.i.d. for seven days | LDP antitussive impact was comparable to the standard DHC treatment | LDP and DHC both had a similar number of patients (n=6) and patients (n=4) reporting side events. However, compared to DHC group (22%), the percentage of patients who reported somnolence in the LDP group (8%) was much lower. |
| Catena 1997 23 | RCT (double-blind) | 209 | 18–75 | Dextromethorphan (DXM) | Moderate non-productive cough | Oral administration t.i.d. for five days | Significant reduction in cough frequency with both treatments; LDP significantly more effective in reducing nocturnal awakenings | The number of patients reporting AEs was significantly higher (P<0.05) in the DXM (12.1%) than in the LDP (3.6%) group |
| Allegra 1988 22 | RCT (double-blind) | 174 | >13 | Placebo (two studies) Morclofone 1% (2 studies) Cloperastine drops 2% (two studies) | Bronchitis cough | Oral administration t.i.d. for three days | LDP was shown to be effective in approximately 80% of patients. The cough frequency was reduced by 33-51% in responder. LDP antitussive activity was shown to be greater than placebo, morclofone, and comparable to cloperastin. | LDP was generally well tolerated and mild side-effects were reported for only 3% of patients. |
| In pediatric patient | ||||||||
| Zanasi et al 2016 31 | Prospective observational study | 330 | 0.4-14 | Antibiotic regimen | Acute cough caused by URTI | Treatment given for six days | The resolution of cough was significantly higher with LDP than with antibiotics | No relevant AEs reported |
| De Blasio 2012 27 | Observational study | 433 | 6.1 | cloperastine/ codeine | Acute cough associated with a URTI | Given for six days | Cough severity reduced by all antitussives | Codeine induced sedation reported |
| Kim 2002 28 | RCT double-blind, two parallel groups | 77 | 3 | DXM | Acute or chronic bronchitis with non-recurrent or slightly recurrent cough | Oral administration t.i.d. for three days | Improvement in cough frequency and severity significantly higher with LDP | Sedation reported in DXM group |
| Banderali 1995 29 | RCT double-blind, double- dummy,two parallel groups, | 267 | 2-14 | Dropropizine | Non-productive cough | Oral administration t.i.d. for three days | Significant decrease in cough frequency and night awakenings with both treatment | Somnolence was reported twice in dropropizine group |
| Fiocchi et al. 1991 32 | RCT double-blind trial | 12 | 2- 8 | None | Asthmatic cough | Oral administration of LDP single dose for four weeks | Significant improvement in nocturnal awakening reduction observed with LDP | Not stated |
Paediatrics
Table 1summarizes efficacy of levodropropizine in paediatric patients. Cough may have a long-lasting effect on the health of children; thus, it may impact their HRQoL. Therefore, despite the possibility of side effects from the use of unsuitable or unnecessary cough drugs, great attention is given on the early management of cough. Paediatric cough treatment often uses two class of antitussive medications: centrally acting medicines and peripherally acting antitussive drugs.12, 18 Due to the limited number of clinical trials in the paediatric population and considering their different clinical endpoints, uses of antitussive agents in children are not supported by adequate efficacy outcomes.12 In recent years, the efficacy of most antitussive drugs, particularly centrally acting cough suppressants has been challenged due to lack of efficacy evidence and increasing reports of association with serious adverse events in children.25
In a clinical investigation conducted by Mannini et al., it was demonstrated that levodropropizine does not have a central depressive impact and had no effect on the hyper ventilatory response to hypercapnia. The study findings supported the peripheral action and good safety profile of levodropropizine, especially in children.18,26 The efficacy of antitussive drugs in reducing the severity of acute cough was evaluated in an observational study conducted by De Blasio et al in 433 paediatric patients. In this study, a higher cough resolution was observed for levodropropizine than with central antitussives. (47% vs. 28% respectively, p = 0.0012).27
Levodropropizine and dextromethorphan were compared for effectiveness in a double-blind, two-parallel groups, randomized controlled trial by Kim et al. in 77 children with bronchitis and non-recurrent or mildly recurrent cough. Levodropropizine significantly reduced cough frequency and severity more than dextromethorphan after two to three days of dosing.
Furthermore, the overall efficacy score with levodropropizine compared to dextromethorphan was significantly greater, indicating a much more beneficial anti-tussive effectiveness of levodropropizine than dextromethorphan.28
In a double blind, double dummy two parallel groups, randomized study carried out by Banderali et al. to evaluate the efficacy of levodropropizine vs central antitussive dropropizine in 258 children for non-productive cough treatment. The study findings showed that both levodropropizine and dropropizine reduced the frequency of coughing fits and nighttime awakenings.29
Evidence from meta-analyses
Zanasi et al. reported a meta-analysis that evaluated the pooled estimates of efficacy in adults and children. This meta-analysis comprising three double-blind RCTs with 389 adult patients compared the antitussive activity of levodropropizine compared to central antitussive drugs. The results showed significant difference in overall efficacy in favour of levodropropizine as compared to centrally active antitussive agent.11 The overall antitussive efficacy of levodropropizine vs. controls reported as standardized mean delta with 95% between confidence interval between treatment groups (−0.176, (−0.282 −0.069) p=0.0015).11
In this meta-analysis for paediatric patients, four studies with 789 children were included in which levodropropizine was compared with central antitussive in three studies 27, 28, 29 and one study against a placebo.32 The results showed that levodropropizine statistically significantly improved the cough severity and nocturnal awakenings results compared to central antitussive drugs in children. These findings support levodropropizine favourable benefit/risk profile in treating cough in paediatric patients.30
Safety profile
A safe and effective antitussive therapy remains a significant area of unmet need for cough management. The safety profile of centrally acting antitussive drugs raises greater safety concerns and present an unacceptable risk–benefit profile for use because of the potential for excessive sedation, a higher risk of developing toxic effects such as life-threatening respiratory depression.12, 33 The lack of a central depressant action by levodropropizine support the favourable safety profile of levodropropizine especially in children.18 The safety profile of levodropropizine compared with codeine was evaluated by Lee et al. in 88 adult patients with chronic Cough. The study reported the frequency of treatment-emergent adverse events was substantially higher in the codeine group than in the levodropropizine group (44.4% vs. 14.0%, P = 0.002). Four of the 20 patients who experienced adverse effects from the drug codeine discontinued their treatments as a result. (Figure 1).30
Figure 1.Treatment emergent adverse event in levodropropizine group compared with codeine 30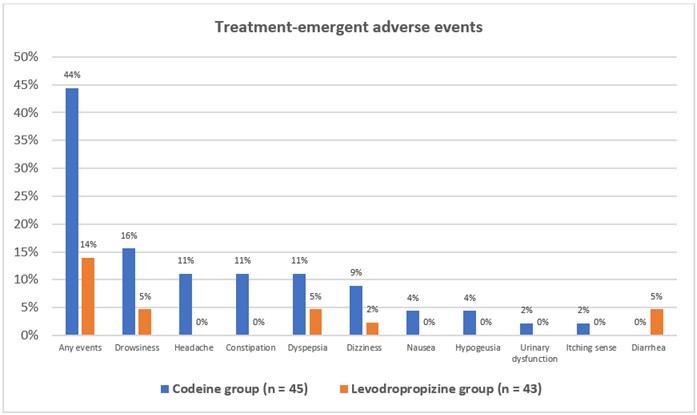
The Tolerability evaluation of levodropropizine compared with dextromethorphan by Catena et al. in 209 adult patients showed that patients reporting adverse events were significantly greater in the dextromethorphan (12.1%) group compared to the levodropropizine (3.6%) group (P<0.05). The overall tolerability assessments indicate a more favourable benefit/risk profile of levodropropizine as compared to dextromethorphan.23 A summary of published clinical study evaluating safety outcome of levodropropizine are summarized in Table 1.
Impact on patients’ HRQoL
Cough is one of the most frequent symptoms that can affect the patients' HRQoL by inducing nausea and sleep disturbance. In an observational study conducted by Blasio et al., the impact of cough on quality of sleep and children’s activities was evaluated using paediatric cough questionnaire (PCQ), developed by the Italian Society of Cough Study. This study included 433 children with a mean age of 6.1 years who had acute cough caused by a URTI. The study result reported the significantly higher cough resolution proportion in the levodropropizine group compared to the central antitussives group (47% vs. 28%, respectively, p = 0.0012), and there was also a notable reduction in irritability and an improvement in their general health (Figure 2).27,34 A total of 60 adult patients with acute cough enrolled in a randomized controlled trial conducted by Alifer et al. to compare the HRQoL of the patients after receiving levodropropizine to a control. The study findings showed that the physical component of HRQoL significantly improved in the levodropropizine group compared to the control group. (Figure 3).35
Figure 2.Impact of cough resolution on children treated with antitussive 27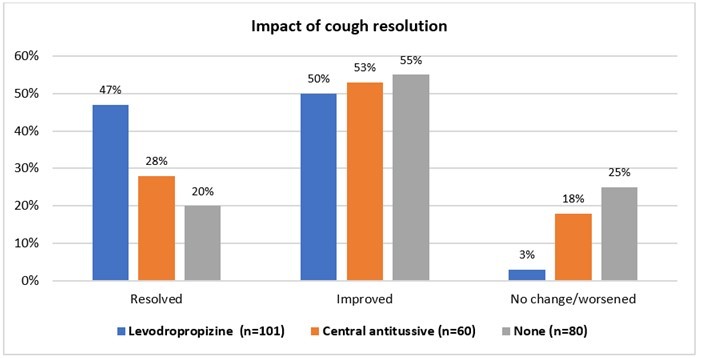
Figure 3.QoL of the patients after receiving levodropropizine to a control 35
Role of levodropropizine in management of COVID 19 related cough
Cough is one of the most common symptoms of COVID-19 which can persist for weeks or months after SARS-CoV-2 infection. The management of cough-related symptoms in COVID-19 patients requires an evidence-based therapeutic approach.36 Zaitsev et al. carried out an open observational multi-center trial to compare the efficacy and tolerability of levodropropizine to conventional medications (mucolytic agent e.g., ambroxol) for the treatment of cough in COVID-19 patients. A total of 250 patient COVID 19 participants who complained of a non-productive cough were enrolled in the study. Significant differences were found in the levodropropizine group between baseline and day four in terms of a significant reduction in the severity of daytime cough (p = 0.002). Although the comparison group also showed positive outcomes, but significant differences were seen only between the baseline and day 8 at night (р = 0.001). The study reported that levodropropizine has demonstrated good efficacy and safety in the treatment of dry, non-productive cough in comparison to standard symptomatic therapy starting on the fourth day.37
Wu et al. used computational methods to investigate the levodropropizine as therapeutic targets for SARS-CoV-2. The screening results suggested that levodropropizine may have a high binding affinity to papain-like protease (PLpro) and may be useful in the treatment of SARS-CoV-2. However, in vivo evaluations of both potency and toxicities of such inhibitors are required before using them against SARS-CoV-2.38 The clinical parameters during the observation period at baseline, day 4 and 8 in patients included in the study shows in Figure 4.
Figure 4.Clinical parameter of levodropropizine group vs control at different timepoint 38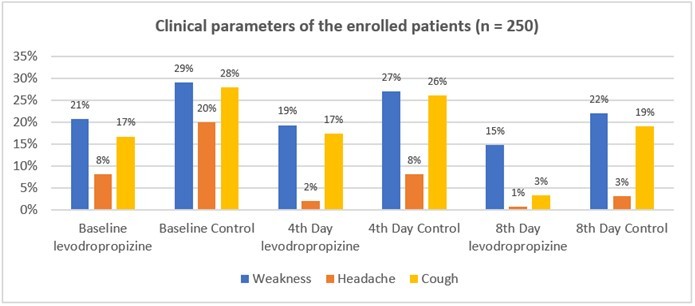
Discussion on recommended treatment strategy for cough
The comparative analysis reported in the efficacy section above for peripherally acting antitussive levodropropizine was found to be safer and more effective to manage the cough. These findings are also consistent with current international recommendations, which recommend the use of peripherally acting antitussive such as levodropropizine for management of cough.5 The ACCP guidelines recommend the use of levodropropizine in adult patients with chronic or acute bronchitis for the short-term symptomatic relief. These guidelines recommended that centrally acting antitussive medications like codeine and dextromethorphan have lower levels of benefit when use to treat acute or chronic bronchitis than levodropropizine (Level of evidence, good; benefit, substantial; grade of recommendation, A).39 Cough is frequently a very distressing symptom that has a significant effect on children's health. Because of the potential for severe sedation, most cough suppressants use by adults have an unfavourable risk-benefit profile for usage in children.18 The use of OTC medications and centrally acting antitussive treatments on paediatric patients with colds and coughs has been challenged by the regulatory bodies such as the United States’ Food and Drug Administration and the United Kingdom’s Medicines and Healthcare products Regulatory Agency. Additionally, the American Academy of Paediatrics has advised against treating children's coughs with dextromethorphan and codeine due to their sedative profile. Respiratory depression slowed or difficult breathing are the most common side effects associated with use of centrally acting antitussive drugs in children. 40,41 The Italian Society of Pediatric Allergy and Immunology advised the use of peripherally acting antitussives such levodropropizine for children and adolescents with cough.16 Indian Environmental Medical Association (EMA) also developed an evidence-based graded clinical guideline to provides recommendation for the management of acute or chronic cough. Risk factors, including smoking, should be addressed in chronic bronchitis (CB) with normal lung function. When compared to dextromethorphan, levodropropizine has a superior benefit/risk profile and can be used to treat such situations. (Level IIB, Strong). 42 EMA has advised the use of antitussives including dextromethorphan, levodropropizine, and levocloperastine for the management of dry cough associated with acute bronchitis case (Level IIB, Strong).42 EMA has also advised to use levodropropizine in non-productive cough associated with primary or metastatic lung cancer (Level IIB; Strong), cough variant asthma (Level IIIC; weak), pulmonary tuberculosis (Level IVB, Strong) and URTI (Level IIB, Strong).42 Although this review provides overall evidence on the efficacy and safety of levodropropizine in both paediatric and adult patients, number of studies in each category of cough medications require further evidence generation with larger sample size, different treatment type, dosing, treatment duration & comparative studies of different antitussives.
Conclusion
Cough is frequently treated using symptomatic drugs. The use of peripheral antitussive agents over centrally acting antitussive agents has increased significantly in recent years, but despite the available evidence, these findings have yet to be translated into clinical practice in India. The usage of currently available cough medications is greatly limited by their central depressing action and frequent side effect. Among the current available drugs, levodropropizine appears to be unique in acting on the sensory fibers and has proven efficacy in cough control with an evident lack of central depressant action. Studies undertaken as part of this review for levodropropizine show that this antitussive agent is effective and well tolerated in the management of cough in patients of all ages, thus further reinforcing the favourable benefit-risk profile of levodropropizine in patients of all ages.
Source(s) of support
The review article manuscript writing charges and article processing charges are funded by Dr Reddy’s laboratories.
Acknowledgements
The review article manuscript writing charges and article processing charges are funded by Dr Reddy’s laboratories.
References
- 1.Francesco A, Marina A, Giuseppina B, Ernesto C, Alfredo C. (2018) Cough, a vital reflex. Mechanisms, determinants and measurements. Acta Bio Medica: Atenei Parmensis. 89(4), 477.
- 2.Sharma S, M F Hashmi, M S Alhajjaj. (2018) . , Cough. In: StatPearls. Treasure Island (FL): StatPearls
- 3.Braman S S. (2006) Postinfectious cough: ACCP evidence-based clinical practice guidelines. , Chest 129(1), 138-146.
- 4.Lai K, Shen H, Zhou X, Qiu Z, Cai S et al. (2018) Clinical practice guidelines for diagnosis and management of cough—Chinese Thoracic Society (CTS) Asthma Consortium. , Journal of Thoracic Disease 10(11), 6314.
- 5.Holzinger F, Beck S, Dini L, Stöter C, Heintze C. (2014) The diagnosis and treatment of acute cough in adults. , Deutsches Ärzteblatt International 111(20), 356.
- 6.S P Galant. (1991) Chronic cough--the spectrum and frequency of causes, key components of the diagnostic evaluation and outcome of specific therapy. , Pediatrics 87(6), 1008-1009.
- 7.Kohno S, Ishida T, Uchida Y, Kishimoto H, Sasaki H et al. (2006) Committee for the Japanese Respiratory Society Guidelines for Management of Cough. The Japanese Respiratory Society guidelines for management of cough. Respirology. , (Carlton, Vic.) 11, 135-186.
- 8.Mahashur A. (2015) Chronic dry cough: Diagnostic and management approaches. Lung India:. , Official Organ of Indian Chest Society 32(1), 44.
- 9.Smith S M, Schroeder K, Fahey T. (2014) Over‐the‐counter (OTC) medications for acute cough in children and adults in community settings. Cochrane Database of Systematic Reviews. 11.
- 10.P C On. (2020) Updates in treatment of adults with chronic cough. , Am J Manag Care 26(11), 239-245.
- 11.Zanasi A, Lanata L, Fontana G, Saibene F, Dicpinigaitis P et al. (2015) Levodropropizine for treating cough in adult and children: a meta-analysis of published studies. , Multidisciplinary Respiratory Medicine 10(1), 1-6.
- 12.P V Dicpinigaitis. (2006) Current and future peripherally-acting antitussives. , Respiratory physiology & neurobiology 152(3), 356-362.
- 13. (2022) Summary of Product Characteristics HACTOSEC. Available from URL:https://www.dafrapharma.com/products/hactosec/.
- 14.Lee S, K Y Nam, Oh J, Lee S, S M Cho et al. (2018) Evaluation of the effects of food on levodropropizine controlled-release tablet and its pharmacokinetic profile in comparison to that of immediate-release tablet. Drug Design, Development and Therapy. 1413-1420.
- 15. (2022) New Drugs Approved by CDSCO. Available from URL:https://cdscoonline.gov.in/CDSCO/Drugs. Accessed on (date).
- 16.A H Morice, Millqvist E, Bieksiene K, S, Dicpinigaitis P. (2020) ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. , European Respiratory Journal 55(1).
- 17.Birring S, F de Blasio, P V Dicpinigaitis, Fontana G, Lanata. (2019) Antitussive therapy: A role for levodropropizine. , Pulmonary pharmacology & therapeutics 56, 79-85.
- 18.G L Marseglia, Manti S, Chiappini E, Brambilla I, Caffarelli. (2021) Acute cough in children and adolescents: A systematic review and a practical algorithm by the Italian Society of Pediatric Allergy and Immunology. , Allergologia et Immunopathologia 49(2), 155-169.
- 19.Melillo G, Malandrino S, Rossoni G, Caselli G, Bestetti A. (1988) . General pharmacology of the new antitussive levodropropizine. Arzneimittel-Forschung/Drug Research 38-42.
- 20.Jeon S, Lee J, Hong T, Paek J, Han S. (2013) Pharmacokinetics and Safety of Levodropropizine Controlled Release Tablet after Repeated Dosing in Healthy Male Volunteers. , Journal of Korean Society for Clinical Pharmacology and Therapeutics 21(2), 113-119.
- 21.Borsa M, Glavenna G, M P Ferrari, Canali S, Giachetti C. (1991) Linearity of levodropropizine, a new antitussive drug, in the healthy volunteer. , European Journal of Drug Metabolism and Pharmacokinetics 178-184.
- 22.Allegra L, Bossi R. (1988) Clinical trials with the new antitussive levodropropizine in adult bronchitic patients. , Arzneimittel-forschung 38(8), 1163-1166.
- 23.Catena E, Daffonchio L. (1997) Efficacy and tolerability of levodropropizine in adult patients with non-productive cough. Comparison with dextromethorphan. Pulmonary pharmacology & therapeutics 10(2), 89-96.
- 24.Luporini G, Barni S, Marchi E, Daffonchio L. (1998) Efficacy and safety of levodropropizine and dihydrocodeine on nonproductive cough in primary and metastatic lung cancer. , European Respiratory Journal 12(1), 97-101.
- 25.S H Lam, Homme J, Avarello J, Heins A, Pauze D. (2021) Use of antitussive medications in acute cough in young children. , Journal of the American College of Emergency Physicians Open 2(3), 12467.
- 26.Mannini C, Lavorini F, Zanasi A, Saibene F, Lanata L. (2017) A randomized clinical trial comparing the effects of antitussive agents on respiratory center output in patients with chronic cough. , Chest 151(6), 1288-1294.
- 27.F De Blasio, P V Dicpinigaitis, B K Rubin, G De Danieli, Lanata L. (2012) An observational study on cough in children: epidemiology, impact on quality of sleep and treatment outcome. , Cough 8(1), 1-6.
- 28.Kim D S, MHMD Sohn, Jang G C. (2002) Levodropropizine in children with bronchitis. , Diagn Treat 22, 9.
- 29.Banderali G, Riva E, Fiocchi A, C I, Giovannini M. (1995) Efficacy and tolerability of levodropropizine and dropropizine in children with non-productive cough. , Journal of international medical research 23(3), 175-183.
- 30.S P Lee, S M Lee, B J Lee, S Y Kang. (2022) Effectiveness and Safety of Codeine and Levodropropizine in Patients With Chronic Cough. , Journal of Korean Medical Science 37(36).
- 31.Zanasi A, Lanata L, Saibene F, Fontana G, Dicpinigaitis P. (2016) Prospective study of the efficacy of antibiotics versus antitussive drugs for the management of URTI-related acute cough in children. Multidisciplinary respiratory medicine. 11, 29.
- 32.Fiocchi A, Arancio R, Murgo P, Banderali G. (1991) Levodropropizine effectiveness on nocturnal cough in asthmatic children. , Eur Res J 4(14), 594.
- 33.P V Dicpinigaitis. (2011) Cough: an unmet clinical need. , British journal of pharmacology 163(1), 116-124.
- 34.F De Blasio, P V Dicpinigaitis, G De Danieli, Lanata L, Zanasi A. (2012) Efficacy of levodropropizine in pediatric cough. , Pulmonary Pharmacology & Therapeutics 25(5), 337-342.
- 35.Alifer O. (2018) Levodropropizine for cough treatment in adults: a randomized controlled trial. , Psychosomatic Medicine and General Practice 3(3), 030361-030361.
- 36.W J Song, C K Hui, J H Hull, S, McGarvey L. (2021) Confronting COVID-19-associated cough and the post-COVID syndrome: role of viral neurotropism, neuroinflammation, and neuroimmune responses. The Lancet Respiratory Medicine. 9(5), 533-544.
- 37.Zaicev A A, E V Bolotova, A V Dudnikova, L V Sнulzhenko, Vizel A A. (2022) Results of an open observational multicenter study of the effectiveness and tolerability of levodropropizine in comparison with standard antitussive therapy (real practice) in the treatment of patients with COVID-19. 32(4), 548-557.
- 38.Wu C, Liu Y, Yang Y, Zhang P, Zhong W. (2020) Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods. , Acta Pharmaceutica Sinica B 10(5), 766-788.
- 39.Irwin R S, Baumann M H, Bolser D C, Boulet L P, Braman S S. (2006) American College of Chest Physicians (ACCP): Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest;129: 1S–23S
- 40.F De Blasio, J C Virchow, Polverino M, Zanasi A, P K Behrakis. (2011) Cough management: a practical approach. , Cough 7, 1-12.
Cited by (3)
This article has been cited by 3 scholarly works according to:
Citing Articles:
International Journal of Basic & Clinical Pharmacology (2024) OpenAlex
Journal of Pure and Applied Microbiology (2024) Crossref
Journal of Pure and Applied Microbiology (2024) OpenAlex
Mony Thakur, Khushboo , Ankita Yadav, K. Dubey, T. C. Dakal et al. - Journal of Pure and Applied Microbiology (2024) Semantic Scholar
