Culturally Tailored Nutrition and Lifestyle Intervention can Effectively Reduce the Cardio-Metabolic Risk Factors in Korean Migrants Living in Australia
Abstract
The risk levels of chronic diseases are increasing among Asian migrants in Western countries compared to their origin-country counterparts. This study evaluates the impact of an 8-week nutrition and lifestyle intervention on cardio-metabolic risk factors in Korean migrants living in Melbourne, Australia. Thirty participants aged 32-62 years completed the program. Self-reported food intake and physical activity, anthropometric and blood pressure measurements, and biomarkers of cardio-metabolic risk were assessed. An initial training session and four consequent nutrition advice sessions were provided for all participants. There was a significant reduction in the waist and hip circumferences. Positive changes were also observed in plasma lipid profiles, calcium intake and frequency of physical activities. These findings demonstrate that a culturally appropriate nutrition and lifestyle intervention can be successfully delivered to reduce the cardio-metabolic risk factors and improve the health and wellbeing of Korean adult migrants.
Author Contributions
Academic Editor: Winnie Chan, Specialist Renal Dietitian, Department of Nutrition and Diatetics.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2015 Hyunsin (Hedy) Sung, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Cardiovascular disease (CVD) is a leading cause of death, accounting for about 30% of all global deaths 1.Risk factors associated with CVD include central obesity, elevated plasma cholesterol and glucose levels, hypertension and a sedentary lifestyle 2, 3. These risk factors are potentially modifiable with lifestyle changes to dietary intake and physical activity level.
It has been well documented that an unhealthy lifestyle such as an unbalanced diet and sedentary life is linked with higher mortality rates in Western countries 4. High dietary fat intakes consisted of 60% energy have been associated with a positive energy balance and results in an accumulation of fatty acids in adipose tissue, skeletal muscle and visceral organs such as heart and liver 5.An increased consumption of processed foods and fast-foods, high in energy, fat and simple sugar, is strongly related to the current epidemic of obesity and diabetes 6. Individuals who visited fast-food restaurants more than twice a week gained nearly 5 kg in body weight over 15 years and also had two-fold greater increase in insulin resistance compared with individuals who visited such restaurants less than once a week 6. An “unbalanced” diet is related to an incidence of adverse health outcomes such as dyslipidemia, high blood glucose level, and CVD. A high carbohydrate diet (≥ 72% of total energy) was reported to be associated with higher body mass index (BMI); hypertension; and dyslipidemia 7. Moreover, individuals with a low physical activity level and sedentary lifestyle have shown an increased risk of all-cause mortality including CVD compared with active individuals 8,9. It has been reported that sedentary lifestyle contributes approximately 6% of the CVD burden worldwide. A meta-analysis of 33 studies
showed that the risk of coronary heart disease in individuals with moderate-intensity of physical activity (approx 150 min/week) was 14% lower than sedentary subjects 10.
Asian migrants in Western countries have shown a higher prevalence of chronic diseases such as coronary heart disease, hypertension, obesity and diabetes compared to their origin-country counterparts 11. Hypertensive Korean-Americans showed greater consumption of fast-food compared to their counterparts in Korea 12.Westernised diet has a strong association with high prevalence of lifestyle-related disease 11, 12, 13. Food choice and physical activity patterns can be altered through migration. Japanese-American men had a lower physical activity, a higher prevalence of obesity and diabetes in comparison to their origin-country counterparts 11. Also Korean-American women born and living in the US were three times more likely to be overweight or obese than their origin-country counterparts 14.Song and colleagues 14 suggested that the high prevalence of obesity in Korean-American women may be associated with dietary acculturation such as more fast food and less green vegetables consumption compared to their counterparts. Additionally these migrants, like other Asian migrants, undertook less physical activity than their origin-contry counterparts 11.
Previous studies with community-based, culturally-tailored behavioural interventions among migrants and ethnic minorities in developed countries have reported beneficial health outcomes 15,16. However there are limited studies on nutrition education intervention focused on a combination of eating behaviour and physical activity among Korean migrants worldwide 17,18. The aim of this study was to investigate the effect of an 8-week nutrition and lifestyle intervention focused on improving cardio-metabolic risk factors including central obesity, blood pressure, blood lipids and glucose on Korean migrants in Australia.
Materials and Methods
Participants
Thirty volunteers (25 females, 5 males) aged between 32 and 62 years completed the 8-week nutrition and lifestyle intervention. Inclusion criteria were self-reported Korean, aged between 30-65 years without chronic heart, liver and kidney diseases; severe cognitive impairment; or any terminal illness; and living in Australia for a minimum of one year. Exclusion criteria include acute or chronic progressive illness such as myocardial infarction and infectious disease. The study was advertised via ethnic magazines, newspapers, and an ethnic radio program. All eligible participants received further information about the study and written consent was obtained from all participants (Figure 1. The study was approved by the Victoria University Human Research Ethics Committee (VU HRETH: 11/45).
Study Design and Procedures
This nutrition and lifestyle intervention was conducted by a bilingual facilitator from the same ethnic background as participants to minimize communication and culture barriers. Prior to the intervention, socio-economic information and the behavioural habits of each participant were collected using questionnaires adopted from an Australian Diabetes, Obesity and Lifestyle (AusDiab) study (Diabetes Info 2011). At both baseline and the conclusion of the program, blood samples and a Health and Wellbeing questionnaire (Your Health and Wellbeing SF-36v2 Health Survey) were collected. All participants completed a 3-day (two week days and one day of the weekend) food diary and physical activity record at commencement, and once a fortnight during the 8-week program, and at the conclusion. All participants at the first session were provided a training session on how to determine their food portion size and complete the food dietary. During the 8-week intervention period, individualised nutrition advice was provided on a fortnight basis by one of the investigators, a qualified nutritionist. These sessions included health monitoring, anthropometric and blood pressure measurements, review of food intake and physical activity records.
The individualised nutrition advice was based on evaluation of their 3-day food records and was designed to improve the dietary intake and physical activity. The program was delivered using a set protocol covering overview of cardio-metabolic risk factors, diet-disease connection, adverse health effects of obesity, and advice on lifestyle modification emphasising food intake and physical activities. The initial nutrition education session focused on the national dietary guidelines and led participants to identify their adverse health risk factors and nutritional needs. This promoted individuals to set up their specific goals for behavioural changes. Low caloric foods such as tofu, beans and low fat dairy products and frequent and intensive physical activities were recommended to obese participants. Once a fortnight follow-up nutrition consultation was delivered to reinforce the dietary guidelines, and advice was given as to how to apply them in practice. The criteria of choosing healthier foods (such as those low in sugar and fat) during shopping, cooking and eating out, and the reasonable portion size were also included. Additionally, advice on how to read and interpret nutrition labelling information was provided for healthier options in food choice in line with individuals’ health status. The nutrition advice included dietary recommendations based on both Korean and Australian dietary guidelines 19,20. All participants were advised to add more multigrains and legumes to the rice based traditional Korean diet and to increase vegetables and fruit consumption. Multigrains and legumes are low GI foods and contain high fibers which are beneficial for all populations.
Physical activity level was also considered as a modifiable behaviour for cardiovascular risk. At each session participants with low physical activity (< 3 per week) were advised and monitored to gradually increase their physical activity level with an increase in the duration and the intensity level. Leisure-time physical activities such as brisk walking; jogging; swimming; weight-lifting and stretching were recommmended for at least 30 min a day and three to five times a week.
Anthropometric Measurement and Blood-Pressure
Anthropometric measurements including height, body weight, waist circumference and hip circumference 22,23,24 were taken by a trained nutritionist. Participants attended the clinic at the same time of the day throughout the intervention period. The cut-off criteria for BMI adopted in the study were based on World Health organization recommendations for Asian populations 21. All anthropometric measurements were taken twice, with results representing the average of the two measurements. Individuals were asked to wear light clothing and were barefooted while anthropometrics were measured using standard protocols. BMI was calculated using the formula: BMI = body weight (kg)/ height (m2) 21.
Resting blood pressure was measured using an automated digital sphygmomanometer (Omron T5, Omron Healthcare, Japan). A participant with over 130 mmHg in systolic blood pressure and/ or over 85 mmHg in diastolic blood pressure was determined as having a hypertension 22.
Biochemical Analyses
Blood samples, approximately five millilitres, were taken in heparinised tubes from a cubital vein after at least 10 hours fasting. Blood glucose concentration was determined using a glucometer (MediSense Precision Plus, Abbott Diabetes Care Inc., Australia, 2010). Blood samples were centrifuged at 3000g and 4°C for 10 minutes. Plasma from blood samples was removed and stored at -80°C until analysis. Total cholesterol, triglycerides, and high-density lipoprotein cholesterol (HDL) levels were determined using commercial assay kits (Thermo Fisher, Australia, 2012). The low-density lipoprotein (LDL) cholesterol levels were determined using the Friedewald formula 23. Plasma C-reactive protein (CRP) assay was performed using an automated enzyme immunoassay kit (CRP Human ELISA Kit, Cayman Chemical Company, US, 2012). All procedures were performed using standard protocols and in accordance with manufacturer’s instructions.
Clinical Assessment of Cardio-Metabolic Risk Factors
The 10-year risk of heart attack was estimated at both baseline and post-intervention using the method of the Framingham Heart Study, with obtained data such as age, gender, ratio of total cholesterol/HDL, systolic blood-pressure, smoking history and anti-hypertension medication status 24.
Health, Dietary Intake and Physical Activity Assessments
General health status of participants was assessed using the Health and Wellbeing questionnaire (SF 36v2). The questionnaire was designed to measure domains of health including physical functioning, general health, and mental health perception (Quality Metric Health Outcomes™, US, 2011). Nutrient intakes were assessed using Foodworks (Xyris Professional 2009, Australia Pty Ltd, 2010). To accurately determine the nutrient intake of Korean foods, data derived from the Korean government food composition database (Korea Rural Resources Development Institute 2006; Korea Food & Drug Administration, 2011) and nutrition information taken from commercial packaging were added into the FoodWorks database.
Statistical Analyses
The sample size for the current study (a minimum of 25) was determined by a statistical power analysis, two tailed t-test at the 0.05 significance level for the power of 90% of expected differences in one of the major measured variables of the study i.e., cholesterol based on the study by Kim and Kim 25.
Differences between baseline and post-intervention in the obtained parameters were assessed using the paired t-test. Statistical analyses of changes in anthropometric measurements, blood-pressure, and food intakes at different time points were analysed using SPSS package (version 19, SPSS Inc., Chicago, IL, 2010). A one-way ANOVA and multiple comparisons were performed using a Tukey HSD post-hoc analysis. All data were expressed as mean (± standard deviation) unless otherwise indicated. Probability values of less than 0.05 were considered statistically different.
Results
The general characteristics of participants prior to the intervention are shown in Table 1.
Table 1. General baseline characteristics of participants enrolled in nutrition and lifestyle intervention program (n=30).| % of participants | ||
|---|---|---|
| Demographics | ||
| Age (year) 44.3 (8.7)† | Age 30- 49Age 50- 65 | 6040 |
| Sex | FemaleMale | 8317 |
| Marital status | MarriedMarried (living alone)Single (divorced, widowed, or never married) | 77717 |
| Length of residence in Australia, year10.5 (7·6)† | < 55 - 910-19≥ 20 | 30272320 |
| Body mass index (kg/ m2)‡23.0 (3.2)† | < 18·5 (Underweight) 18·5 - 22·9 (Normal)23 – 24·9 (Overweight)≥ 25 (Obese) | 3532023 |
| Health behaviours | ||
| Smoking Status | Non-smokerPast smokerCurrent smoker | 702010 |
| Alcohol intake Status | Non-DrinkerDrink:1-2/weekDrink:3-4/weekDrink:≥ 5/week | 43371010 |
| Exercise Status Exercise session (30min) per week2.7 (1.7)† | None1 session2-3 sessions4 sessions5 sessions or more | 401372020 |
After the 8-week nutrition and lifestyle intervention, both waist circumference and hip circumference fell significantly (1.4 cm and 0.8 cm respectively, Table 2) although there were no significant changes in body weight, BMI, waist-hip ratio, or blood pressure.
Table 2. Anthropometric Measurements and Blood-Pressure of Participants at Baseline and Post-intervention (n=30).| Week 0 | Week 8 | Average change | |
| Body weight (kg) | 60.3 (10.1) | 60.3 (9.5) | 0 |
| BMI (kg/m2) | 23.0 (3.2) | 23.0 (3.1) | 0 |
| Waist circumference (cm) | 77.4 (9.4) | 76.0 (9.0)* | -1·4 |
| Hip circumference (cm) | 94.9 (5.5) | 94.1 (5.1)* | -0·8 |
| Waist-hip ratio | 0.813 (0.07) | 0.806 (0.07) | 0 |
| Systolic blood-pressure (mmHg) | 119 (17.4) | 118 (15.1) | -1.7 |
| Diastolic blood-pressure (mmHg) | 75 (9.7) | 72 (12.7) | -3.2 |
Average blood glucose, plasma total cholesterol, and LDL at commencement of the program were in the borderline of cardio-metabolic risk. After 8-week intervention, total cholesterol reduced significantly from 6.0 to 5.1 mmol/L (Figure 2). A marked improvement in both LDL and HDL was also recorded. LDL reduced from 4.8 to 3.3mmol/L (P < 0.001) and HDL increased from 1.1 to 1.7 mmol/L (P < 0.001). Although not statistically significant, CRP dropped slightly from 1.5 ± (0.9) mg/L to 1.3 (1.1) mg/L over the program period. The average risk level for 10-year heart attack was dropped by half from the baseline (2.4%). The general health assessment including physical and mental health showed a trend of improvement although it was not statistically significant.
Figure 2.Changes in cardio-metabolic biomarkers after 8-week intervention (n=29).BGL, blood glucose level; LDL, low-density lipoprotein cholesterol; HDL, high-density lipoprotein cholesterol, TG, triglyceride.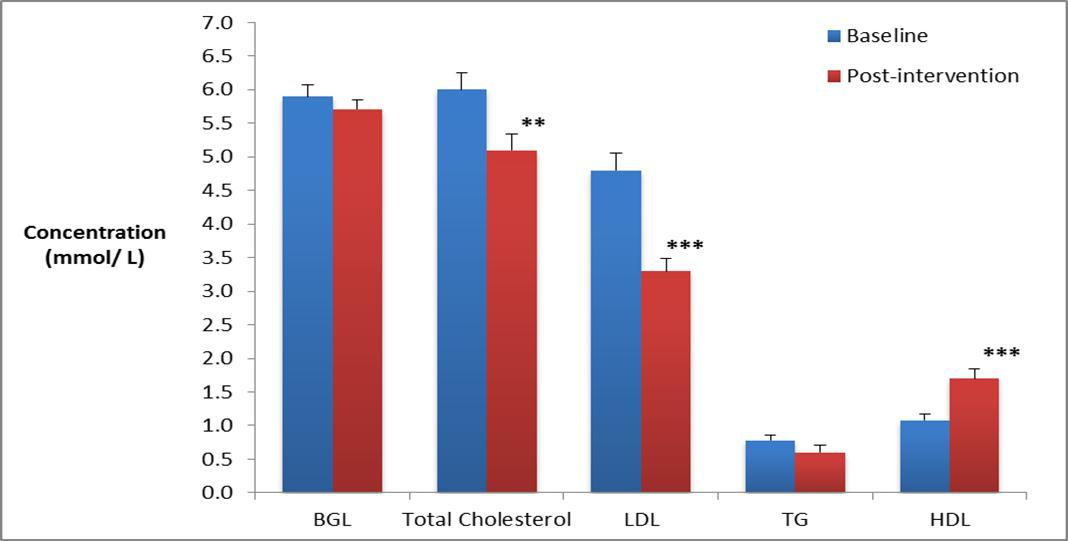
Values are expressed as mean (SD).
*P < 0.005;
** P < 0.001.
Food intake analysis showed a significant increase in calcium intake over the intervention period (Table 3). There were no significant changes observed in total daily energy intake and energy contribution from carbohydrate, protein and fat. The average weekly exercise sessions were increased from 2.7 (1.7) at baseline to 4 (1.2) after week 4 (P < 0.001) and remained steady until week 8.
Table 3. Daily food intakes over 8-week intervention period (n=30).| Week 0 | Week 4 | Week 8 | |
| Energy intake (kJ) | 6330 (1880) | 6570 (1930) | 6400 (1390) |
| Carbohydrate (%)† | 53 (7) | 53 (9) | 53 (7) |
| Protein (%)† | 20 (6) | 19 (4) | 20 (3) |
| Fat (%)† | 25 (6) | 26 (6) | 25 (7) |
| Saturated fatty acid (%)† | 8 (3) | 9 (3) | 9 (3) |
| Alcohol (%)† | 2 (6) | 3 (5) | 1 (6) |
| Monounsaturated fatty acids (g) | 14.1 (6.7) | 15.1 (8.3) | 14.9 (6.4) |
| Polyunsaturated fatty acids (g) | 7.5 (2.7) | 8.4 (4.1) | 8.8 (4.6) |
| Calcium (mg) | 507 (242) | 691 (288)* | 633 (263)* |
| Sodium (g) | 2.0 (0.9) | 2.2 (0.8) | 2.1 (0.9) |
| Fibre (g) | 20 (9) | 22 (9) | 22 (11) |
Discussion
One of the main findings of this study was the significant decline in waist circumference after the 8-week nutrition and lifestyle intervention although no significant changes in BMI or body weight were observed. These results were consistent with the study by Colkesen et al. 26 in that a 2 cm reduction in waist circumference was observed with no change in BMI over a 7-month period.
The decline in waist circumference found in the present study has a significant implication for management and prevention of CVD and other lifestyle-related diseases 3, 27. Waist circumference is a useful and convenient measure of central obesity, and it has been reported to have a strong association with the total body fat (%). Central obesity is considered as one of the primary risk factors for CVD, particularly in Asian populations 28. Previous studies have found that high body fat in Asian population is strongly associated with CVD risk 27, 28, 29. A higher proportion of body fat has been reported among Asians although their BMI is usually lower than Caucasians 27, 28.
The cause for the significant reduction in waist circumference independent of body weight may be related to differential response of adipose tissues to lipolysis consequent to changes in dietary intake and/or physical activity 30.Improved dietary intake, in particular increased calcium consumption, may also contribute to the reduction in waist circumference. Intake of high calcium dairy products was closely associated with reduction in waist circumference 31. A calcium-rich diet without energy restriction for 24 weeks resulted in a decrease in total body fat, abdominal fat, and an increase in lean mass without significnat changes in body weight whereas a low calcium diet group did not show significant changes. Zemel et al. and and Shi et al. suggested that a high-calcium diet decreases calcitriol level and that in turn inhibits intracellular Ca2+ level, stimulating lipolysis and inhibiting lipogenesis, and leading to loss of body fat 31, 32. The reduction of waist circumference in the current study is probably associated with increased calcium intake from dairy products. At baseline the daily average calcium intake was 507 mg and it was increased to 691 mg in week 4 and then 633 mg in week 8. The waist circumference is reflective of abdominal fat. Large waist circumference is strongly associated with increased chance of developing cardio-metabolic disorders particularly in Asian populations 28.
Our study also showed significant improvement in blood lipid profiles parallel to the improvements in waist circumference. After 8-week intervention, total cholesterol and LDL were reduced to the desirable range. This was in agreement with a 24-week lifestyle intervention study on Pakistani female migrants in Australia 15. Although not statistically significant there was a slight reduction in triglyceride after the 24-week intervention. Previous study showed that triglyceride in Pakistani female migrants remained steady after 12-week lifestyle intervention but reduced significantly after 24-week 15. This suggests that a longer lifestyle intervention period might be required for significant improvement of triglyceride level.
HDL is inversely correlated with atherosclerotic conditions including myocardial infarction and stroke 33. HDL can promote cholesterol efflux from peripheral cells and carries cholesterol back to the liver through the selective uptake and subsequent metabolism of cholesterol 33. The improvement in cholesterol profiles at the end of intervention is of significance to the cardiovascular health, in particular to the Korean population concerned in this study. The Korean National Health and Nutrition Examination Survey between 1998 and 2007, reported that low HDL level was the most common component among the cardio-metabolic risk factors in Koreans, followed by central obesity and elevated triglyceride 34, 35. According to the report Koreans have increased the prevalence of central obesity, elevated triglyceride and blood glucose concentration; and a decreased HDL over the last decade. The increase in those modifiable risk factors for CVD can adversely affect populations unless they are corrected via behavioural modification.
A waist circumference indicative of central obesity is linked with a chronic inflammatory state 36. C-reactive protein (CRP) has been commonly used in recent years as a biomarker for inflammation 33. A study on CVD risk factors among healthy, middle-aged women observed that waist circumference had a strong association with CRP 36. Women, who subsequently developed cardiovascular disorders, had approximately two times higher CRP level than their counterparts without vascular diseases 37. Those with the highest CRP level had a five times increase in risk of vascular disorders and a seven times increase in relative risk of future CVD. Therefore abdominal fat deposition is suggested as the most important factor contributing to inflammation, resulting in a high level of CRP and higher risk of CVD 37. In the present study, although not statistically significant, the CRP concentration dropped slightly over the intervention period parallel to the decline of waist circumference 36. This indicates an improvement in the state of chronic inflammation, a major component of pathophysiology of atherosclerosis.
In relation to improved lipid profiles this nutrition and lifestyle intervention may be ideally facilitated to modification of lifestyle. Other studies have shown that participation in structured exercise programs reduces cardio-metabolic risks. Moderate exercise is beneficial in modifying components of CVD, including promoting loss of central fat accumulation, increasing muscle mass, reducing blood pressure and triglyceride and increasing HDL 34, 38. The increased exercise did not lead to significant changes in body weight in the current study maybe due to that large proporation of participants had a normal range of body weight at the baseline, or it could also be attributed to the increase in lean body mass paralled with the reduction in body fat after eight week intervention.
The average level for 10-year CVD risk showed a significant reduction by 1.2% over the program period. This outcome is mainly attributed to improvement in blood pressure and significant changes in total cholesterol and HDL. Similarly Kousar et al. in a 12-week lifestyle intervention study demonstrated favourable changes in cardio-metabolic markers 15.
The dietary pattern in the present study was similar to that of Koreans in America in that a lower carbohydrate and sodium intakes but higher fat intakes were observed compared to their counterparts living in Korea 39. The lower daily sodium intake in Korean migrants was suggested to be correlated with dietary habit changes after immigration as they tended to consume less frequently traditional Korean foods 40. Reduced sodium intake has potential health benefits. It is well known that sodium intake is strongly linked to blood pressure regulation with decreased sodium intake being strongly associated with reduction in systolic blood pressure 41. Clinical trials have demonstrated that reduced salt intake lowers blood pressure in participants at risk of metabolic syndrome 42.
The most significant dietary improvement after 8-week nutrition and lifestyle intervention was the consumption of dairy foods (mostly low fat milk and yoghurt) and that resulted in the remarkable increase in calcium intake. Increased calcium intake improves the bone health particularly in women 20.There were also slight increases in the consumption of monounsaturated fatty acids and polyunsaturated fatty acids, and dietary fibres which was consistent with a previous community-based nutrition study 43. Polyunsaturated fatty acids (PUFA) are associated with lower incidence of CVD and several other lifestyle-related diseases 44. High PUFA such as omega-3 fatty acids consumption was found to be associated inversely with LDL and positively with HDL cholesterol 45 that may contribute to the improvement in both LDL and HDL in the present study.
Conclusions
The present study demonstrated that an 8-week nutrition and lifestyle intervention with modification of dietary intake and increased physical activities was effective on cardio-metabolic risk prevention. The results highlight the clinical efficacy of a culturally appropriate intervention that leads to an improvement in risk factors associated with cardiovascular disease including waist circumference, LDL and HDL levels. The nutrition and lifestyle intervention would be a reasonable approach to reduce the prevalence of cardio-metabolic diseases. This program could also be useful for other ethnic groups. However there were limitations in this study such as relatively small subject number and lack of gender balance.
Acknowledgements
We wish to thank all the participants of this project for their cooperation and effort. We also thank the late Mrs Dawn Bannon and Mrs Kristina Nelson for their assistance with blood collection. We greatly appreciate the valuable comments from Prof. Duo Li.
References
- 1. (2011) Global status report on noncommunicable diseases 2010 [Internet]. World Health Organization. cited
- 2.Kim M T, Juon H S, Hill M N, Post W, Kim K B. (2001) Cardiovascular disease risk factors in Korean American elderly. , Western Journal of Nursing Research 23(3), 269-82.
- 3.Després J-P, Lemieux I, Bergeron J, Pibarot P, Mathieu P et al. (2008) Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arteriosclerosis, Thrombosis, and Vascular Biology. 28(6), 1039-49.
- 4.Andersson H I.Increased mortality among individuals with chronic widespread pain relates to lifestyle factors: a prospective population-based study. , Disability & Rehabilitation 31(24), 1980-7.
- 5.Schrauwen P.High-fat diet, muscular lipotoxicity and insulin resistance. Proceedings of the Nutrition Society 66(01), 33-41.
- 6.Pereira M A, Kartashov A I, Ebbeling C B, L Van Horn, Slattery M L et al.Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. , The Lancet 365(9453), 36-42.
- 7.Park S-H, Lee K-S, Park H-Y.Dietary carbohydrate intake is associated with cardiovascular disease risk in Korean: Analysis of the third Korea National Health and Nutrition Examination Survey (KNHANES III). , International Journal of Cardiology 139(3), 234-40.
- 8.Qi Q, Li Y, Chomistek A K, Kang J H, Curhan G C et al. (2012) Television watching, leisure time physical activity, and the genetic predisposition in relation to body mass index in women and men / clinical perspective. Circulation. 126(15), 1821-7.
- 9.Lee I-M, Shiroma E J, Lobelo F, Puska P, Blair S N et al.Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. The Lancet. 380(9838), 219-29.
- 10.Sattelmair J, Pertman J, Ding E L, Kohl H W, Haskell W et al.Dose response between physical activity and risk of coronary heart disease a meta-analysis. , Circulation 124(7), 789-95.
- 11.Huang B, Rodriguez B L, Burchfiel C M, Chyou P H, Curb J D et al.Acculturation and prevalence of diabetes among Japanese-American men in Hawaii. , American Journal of Epidemiology 144(7), 674-81.
- 12.Kim M J, Lee S J, Ahn Y-H, Bowen P, Lee H.Dietary acculturation and diet quality of hypertensive Korean Americans. , Journal of Advanced Nursing 58(5), 436-45.
- 13.Whittemore A S, Wu-Williams A H, Lee M, Shu Z, Gallagher R P et al. (1990) physical activity, and colorectal cancer among Chinese. in North America and China. Journal of the National Cancer Institute 82(11), 915-26.
- 14.Song Y J, Hofstetter C R, Hovell M F, Paik H Y, Park H R et al.Acculturation and health risk behaviors among Californians of Korean descent. , Preventive Medicine 39(1), 147-56.
- 15.Kousar R, Burns C, Lewandowski P.A culturally appropriate diet and lifestyle intervention can successfully treat the components of metabolic syndrome in female Pakistani immigrants residing in Melbourne. , Australia. Metabolism 57(11), 1502-8.
- 16.Nicklas B J, Dennis K E, Berman D M, Sorkin J, Ryan A S et al. (2003) Lifestyle Intervention of Hypocaloric Dieting and Walking Reduces Abdominal Obesity and Improves Coronary Heart Disease Risk Factors. in Obese, Postmenopausal, African-American and Caucasian Women. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 1, 2003-58.
- 17.Hwang G S, Choi J W, Choi S H, Lee S G, Kim K H et al.Effects of a tailored health promotion program to reduce cardiovascular disease risk factors among middle-aged and advanced-age bus drivers. , Asia-Pacific Journal of Public Health 24(1), 117-27.
- 18.Islam N, Zanowiak J, Wyatt L, Chun K, Lee L et al.A Randomized-Controlled, Pilot Intervention on Diabetes Prevention and Healthy Lifestyles in the New York City Korean Community. , Journal of Community Health 38(6), 1030-41.
- 19. (2010) The Korean Nutrition Society and Ministry of Heatlh & Welbeing. Deitary Reference Intake For Koreans. Available from: http://www.kns.or.kr/
- 20. (2005) Dietary Guidelines for Australian Adults [Internet]. National Health Medical Research Council. cited 11.
- 21.Health World.Organisation. Obesity: Preventing and managing the global epidemic_Report of a WHO consultation. Australian Psychologist. 2000;WHO Technical Report Series 894
- 22.Expert Panel on.Detection E, and Treatment of High Blood Cholesterol in, Adults y. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel iii). , JAMA 285(19), 2486-97.
- 23.Friedewald W T, Levy R I, Fredrickson D S.Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical chemistry. 18(6), 499-502.
- 24. (2013) Risk assessment tool for estimating your 10-year risk of having a heart attack [Internet]. National Health Medical Research Council. cited
- 25.Kim H-K, Kim M-J.Effects of weight control program on dietary habits and blood composition in obese middle-aged women. , Korean J Nutr 43(3), 273-84.
- 26.Colkesen E B, Ferket B S, JGP Tijssen, Kraaijenhagen R A, van Kalken CK et al.Effects on cardiovascular disease risk of a web-based health risk assessment with tailored health advice: a follow-up study. Vascular health and risk management. 2011-7.
- 27.Deurenberg P, Urenberg-Yap M, Guricci S.Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002, 141-6.
- 28.Kwon S. (2009) Association between abdominal obesity and cardiovascular risk factors in normal-weight Korean women. Health Care for Women International. PubMed PMID: 2010255129. Language: English. Entry Date: 30(5), 447-52.
- 29.Health World.Organisation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. The Lancet. 363(9403), 157-63.
- 30.Cameron A J, Magliano D J, Zimmet P Z, Welborn T, Shaw J E.The Metabolic Syndrome in Australia: Prevalence using four definitions. Diabetes Research and Clinical Practice. 77(3), 471-8.
- 31.Zemel M B, Richards J, Milstead A, Campbell P.Effects of calcium and dairy on body composition and weight loss in African-American adults. , Obesity Research 13(7), 1218-25.
- 32.Shi H, Norman A W, Okamura W H, Sen A, Zemel M B. (2002) 1alpha,25-dihydroxyvitamin D3 inhibits uncoupling protein 2 expression in human adipocytes. Federation of American Societies for Experimental Biology. Nov;16(13): 1808-10. PubMed PMID: 12223452-2002.
- 33.Freeman D J, Norrie J, Caslake M J, Gaw A, Ford I et al. (2002) C-reactive protein is an independent predictor of risk for the development of diabetes in the west of Scotland coronary prevention study. Diabetes. 51(5), 1596-600.
- 34.Grundy S M, Cleeman J I, Daniels S R, Donato K A, Eckel R H et al. (2005) . Diagnosis and Management of the Metabolic Syndrome. Circulation 112(17), 2735-52.
- 35.Lee K. (1998) Cardiovascular risk prevalence, awareness, treatment, and control from. to , Asia Pac J Clin Nutr 19(2), 261-5.
- 36.Ridker P M, Buring J E, Shih J, Matias M, Hennekens C H. (1998) Prospective study of C-reactive protein and the risk of future cardiovascular events among apparently healthy women. Circulation. 98(8), 731-3.
- 37.Heilbronn L K, Noakes M, Clifton P M. (2001) Energy restriction and weight loss on very-low-fat diets reduce C-reactive protein concentrations in obese, healthy women. Arteriosclerosis, Thrombosis, and Vascular Biology. 21(6), 968-70.
- 38.Stewart K J.Exercise training and the cardiovascular consequences of type 2 diabetes and hypertension: Plausible mechanisms for improving cardiovascular health. , JAMA 288(13), 1622-31.
- 39.Park S-Y, Murphy S P, Sharma S, Kolonel L N.Dietary intakes and health-related behaviours of Korean American women born in the USA and Korea: The Multiethnic Cohort Study. Public Health Nutrition. 8(07), 904-11.
- 40.Kim J, Chan M.Acculturation and dietary habits of Korean Americans. , British Journal of Nutrition 2004, 469-78.
- 41.Astell K J, Mathai M L, McAinch A J, Stathis C G, Su X Q.A pilot study investigating the effect ofCarallumafimbriataextract on the risk factors of metabolic syndrome in overweight and obese subjects: a randomised controlled clinical trial. , Complement Ther Med 21(3), 180-9.
- 42.Whelton P K. (1996) Primary prevention of hypertension: rationale, approaches, realities and perspectives. Journal of human hypertension.
- 43.Bernstein M A, Nelson M E, Tucker K L, Layne J, Johnson E et al.A home-based nutrition intervention to increase consumption of fruits, vegetables, and calcium-rich foods in community dwelling elders. , Journal of the American Dietetic Association 102(10), 1421-7.
Cited by (6)
This article has been cited by 6 scholarly works according to:
Citing Articles:
Ghadir Fakhri Aljayyousi, Maher Abu Munshar, Farid al-Salim, Elwidaa Osman - BMC Public Health (2019) Semantic Scholar
BMC Public Health (2019) OpenAlex
BMC Public Health (2019) Crossref
R. Mabry, M. J. Koohsari, F. Bull, N. Owen - BMC Public Health (2016) Semantic Scholar
BMC Public Health (2016) OpenAlex
BMC Public Health (2016) Crossref
International Journal Of Nutrition (2015) OpenAlex
International Journal Of Nutrition (2015) OpenAlex

