Myasthenia and Antisynthetase Antibody Syndrome: A Case Report in Togo
Abstract
Myasthenia is a rare neurological condition with risk of death in case of inappropriate
management. The outcome of this pathology is very bad in developing countries with inadequate technical
Platform. We underlined the main difficulties of diagnostic and the management of Myasthenie and antisynthetase antibody syndrome in a 44 years-old Togolese man.
Author Contributions
Academic Editor: Pengcheng Han, Dignity Health St Joseph Hospital and Medical Center
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2017 GUINHOUYA Kokou Mensah, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Myasthenia gravis is an autoimmune disease of the neuromuscular junction 1. It is a rare condition, with an estimated prevalence between 45 and 142 per 1000 000 inhabitants, which can occur at any age, but with a clear predominance of females 2. Myasthenia gravis may in rare cases associate with other immune diseases such as Hashimoto's thyroiditis, lupus erythematosus, rheumatoid arthritis and juvenile diabetes 3. The association of myasthenia gravis with antisynthetase antibody syndrome is even more rare 4. We report here a case of this association between myasthenia gravis and anti-synthetase syndrome.
Observation
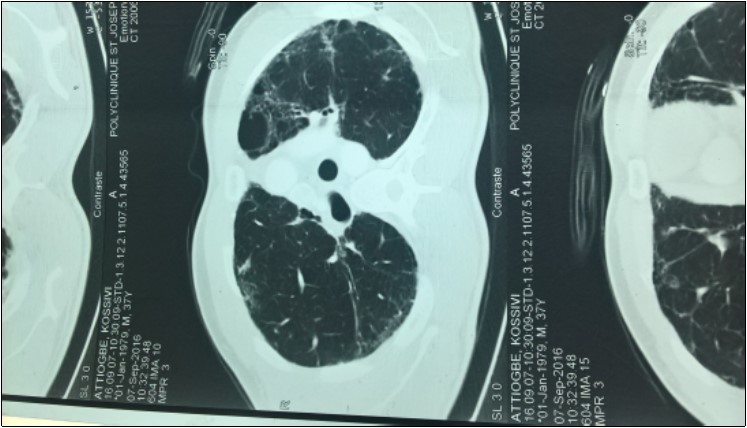
Mr ATT Kos is a 44-year-old patient receiving neurological consultation for dyspnea and sensation of generalized muscle weakness worsening on exertion. The onset of the symptoms dates back to August 2005 marked by the progressive installation of a dyspnea of effort without the notion of cough or slimming. There was no associated infectious context. A consultation in pneumology made it possible to classify his dyspnea at stage I of Sadoul. After a chest radiograph that was normal, he had a thoracic CT scan that revealed multiple bubbles of bilateral emphysema. The patient was then given corticosteroids and beta 2 mimetic. The development was marked by a discreet improvement in dyspnea. The patient again consults with the persistence of dyspnea and a fatigability to the usual effort with modification of the timbre of the voice. This consultation made on December 29, 2016 had made it possible to find episodes of rare false roads as well as a ptosis in case of extreme fatigue. Clinical examination was normal. The diagnosis of myasthenia gravis was then discussed. The detection of anti-receptor anti-acetylcholine antibodies (Ac Anti RACH) was positive with a titre of 0.8 nmol / ml (normal less than 0.2 nmol / ml.) The electromyogram showed a moderate decrease in motor potential at The repetitive stimulation was of the order of 9% .The mediastinum scan showed bilateral pulmonary fibrosis (Figure 1) in relation to its progressive pulmonary pathology and a prostigmine test was performed during a fatigue episode associated with A ptosis and a marked regression of the signs The examination of the patient by a pulmonologist revealed that his present dyspnoea was in Stage II of SAOUL Spirometry reported a 52% FVCI, 63% FEV 1 EFF To 118%, with no improvement in the beta 2 mimetic parameters, and the gasometric data were: PaO2 = 59%, PaCO2 = 54%, PH = 7.39 Hb = 14.3 and HCO3 = 32 The association of myasthenia gravis and fibrosis Motivated by the search for antinuclear antibody: negative; Anti-tRNA-synthetase antibody: positive for anti-PL7 and negative for anti-PL12; Negative also for anti-EJ and anti-OJ. Anti-KU and anti-Pm / Scl antibodies were also negative. Anti-synthetase syndrome has been retained in our patient. It was then placed on Pyridostigmine at progressive dose and Prednisolone at degressive dose. This treatment allowed a stabilization of the clinical state of the patient.
Discussion
Among rare neuromuscular junction conditions, autoimmune myasthenia gravis remains the most common cause. Its prevalence is between 45 and 142 per 1000 000 inhabitants, while its incidence varies from 2.5 to 20. case / million / year depending on the populations studied 2. SAS is part of a heterogeneous group of primary inflammatory myopathies. This syndrome is characterized by the association of inflammatory myopathy, interstitial lung disease, characteristic cutaneous abnormalities such as "mechanic's hands", Raynaud's syndrome, inflammatory arthritis, and Biological, anti autoantibodies specific anti-nuclear called "anti synthetases" which gave their name to the syndrome. The frequency of clinical signs is variable: 94% for inflammatory arthritis, 62% for the phenomenon of Raynaud, 71% for the sign of the mechanic's hand 5. There are currently eight different SASs. It is exceptional to be in the presence of two SAS simultaneously. Depending on the antibody present, the clinical expression of the disease is different 6. Our patient was positive for PL7 antibody. Hervier B et al noted by reporting 17 cases that anti-PL7 positive patients have in 60 to 100% of pulmonary manifestations. This is the case of our patient who had for several years as main symptom a dyspnea of effort. In all cases according to some authors 6, it is necessary to think of looking for an anti-synthetase antibody in an interstitial pneumopathy. Prognosis depends to a great extent on pulmonary involvement. Patients positive for PL12 had skin, vascular (Raynaud's syndrome), pulmonary and esophageal 6. The aforementioned extra pulmonary signs are absent in our patient concordant with the negativity of anti PL12 in the latter. The physiopathology of SAS remains unknown to the present day. Only hypotheses have been suggested, indexing a genetic susceptibility and environmental factors (viral and bacterial infections) that can be an immunologically triggering factor. The mechanism of immune response and antibody production remains unclear 7. The diagnosis of myasthenia gravis was mentioned in our patient before the pharmacological test, the dosage of anti anti RACH. From a therapeutic point of view, anticholinestherases represent the first-line treatment of the symptomatic strand. The background treatment is done with corticosteroids and immunosuppressants. Plasma exchanges and immunoglobulin administration are reserved for severe relapses or myasthenia gravis 2. There are currently no randomized controlled trials in the treatment of SAS 6. However, treatment lines are proposed. In the first line, corticosteroids (CS) at 1 mg / kg / day over a period of 4 to 8 weeks followed by a progressive reduction. In the absence of a response after 12 weeks, immunosuppressive therapy should be combined. Azathioprine is the most widely used drug, as several studies have shown its efficacy in the range of 57-75% at 2 to 3 mg / kg / day. Second-line therapy is the administration of intravenous immunoglobulin (Ig IV), cyclosporine or plasma exchange. However, a randomized, placebo-controlled study showed no benefit to plasma exchange 7. The treatment of myasthenia gravis and SAS containing to some extent the same molecules, we put our patient under anticholinestherasics (Pyridostigmine), corticosteroid (Prednisolone) and immunosuppressant (Azathioprine).We are waiting for a specialist immunological advice that we lack in Togo.
Conclusion:
SAS is rare but should be mentioned before myasthenia gravis with pulmonary manifestations. It would be interesting with the HIV pandemic in Black Africa to systematically investigate possible relationships between HIV infection, possible lung infections and possible myasthenia gravis for better management.
References
- 1.Lindstrom J. (1980) Experimental autoimmune myasthenia gravis. , J Neurol Neurosurg Psychiatry 568-576.
- 2.P Goulon-Goeau C et Gajdos. (2002) Myasthénie et syndromes myasthéniques. Encycl Méd Chir,Neurologie,17-172-B-10.
- 3.Braunwald E, Fauci A S, Kasper D L, Hauser S L, Longo D L et al. (2001) Neurologic disorders. , Principles of Internal Medicine 15, 2518.
- 4.Diaco M, Ancarani F, Montalto M. (2004) Association of myasthenia gravis and antisynthetase Syndrome: a case report. , International Journal of Immunopathology And pharmacology 17(3), 395-399.
- 5.Bergouin C, Bure M, Tavernier J-H, Lamblin C, C A Maurage. (2002) Le syndrome des anti-synthétases. , Rev Mal Respir 19, 371-374.