Abstract
Background:
Conventional transthoracic echocardiography (TTE) and tissue Doppler imaging (TDI) are usually unable to reveal very early subtle abnormalities in left ventricular (LV) systolic function caused by hypertension, prior to manifestation of hypertrophy (LVH). This study was undertaken to assess whether speckle tracking echocardiography (STE) provides more insight into early hypertension induced LV systolic dysfunction, with the purpose of identifying patients at higher risk for heart failure (HF).
Methods:
Fifty patients (54.16 ± 8.4 years) and 50 controls (52.17 ± 8.6 years) were enrolled. According to the presence or absence of LVH, patients were classified as LVH(+) and LVH(–), respectively. Global longitudinal function was calculated by TDI, global strains (longitudinal (LS), radial (RS), and circumferential (CS)) were assessed by STE.
Results:
Conventional TTE showed a normal systolic function in all patients. TDI was able to detect a systolic dysfunction only in the LVH(+) group (P < 0.001) whereas STE revealed an impairment of systolic LS and CS in all patients, including those without hypertrophy (P =<0.0001). Furthermore, in the LVH(+) group, STE showed increased RS .
Conclusion:
In hypertensive patients, STE provides more detailed information than conventional echocardiography and TDI, since it reveals a systolic dysfunction before hypertrophy occurs (Stage A of ACC/AHA classification of HF) and identifies some early LV mechanic changes that might improve the clinical management of these patients
Author Contributions
Academic Editor: Dongmei Wu, Department of BIN Fusion Technology ; Chonbuk National University; South Korea
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2013 Raghvendra Choudhary, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction :
Background:
Hypertension is a well-recognized risk factor for cardiovascular disease and is a major contributor to a large percentage of heart failure (HF) cases.1, 2, 3 Identifying subclinical left ventricular (LV) systolic dysfunction among hypertensives might be helpful in identifying patients at higher risk of developing heart failure.
Also, given the prevalence of hypertension in the population, identifying patients at high risk for heart failure might permit targeted preventive strategies. Early detection of left ventricular (LV) systolic dysfunction in affected patients is, therefore, a crucial issue.
Conventional echocardiography, however, detects abnormalities in LV systolic function only in the advanced stages of hypertensive heart disease (HHD), when a clear LV remodeling/hypertrophy is evident; diastolic LV dysfunction, in contrast, occurs early and its detection is easier even by conventional techniques.4, 5, 6, 7
Nevertheless, recent research on HF with normal ejection fraction (EF) has demonstrated that isolated diastolic dysfunction is rare, being abnormalities of diastolic performance most frequently associated with a subclinical impairment of systolic function.8, 9, 10, 11, 12, 13, 14, 15 In this respect, preclinical alterations of LV systolic function have been demonstrated in patients with essential hypertension and normal EF by tissue Doppler imaging (TDI), strain echocardiography or magnetic resonance tagging.16, 17, 18, 19, 20
It is previously demonstrated that M-mode echocardiography can be used to measure circumferential shortening at the mid-wall (FSmw,%),21, 22 a measure of regional circumferential strain. Reduced FSmw is prevalent among hypertensives with hypertrophic remodeling,21 and de Simone and coworkers have shown that low FSmw in relation to stress is a marker of poor outcome.22 However, FSmw is related to ventricular geometry—the relative wall thickness(RWT).21 Newer methods, such as 2D – speckle imaging, appear to provide a direct, angle and geometry independent measure of circumferential strain (CS).23
Recently, it has been demonstrated that speckle tracking echocardiography (STE) provides more information than TDI, allowing a non invasive measurement of overall LV strain and twist.24, 25, 26, 27 This technique, therefore, can provide new mechanistic insight into systolic dysfunction even in patients without structural cardiac alterations (Stage A of ACC/AHA classification of HF).28
The aim of the current case-control study was to use speckle tracking imaging as well as standard echo techniques to identify subclinical abnormalities in LV function among hypertensives, as compared to normal controls.
Aims and Objectives
To assess the subtle differences in the LV principal strains for characterizing features of subclinical LV dysfunction in patients with systemic hypertension and preserved LV systolic pump function.
Methods
Study Population.
Adult subjects of both genders (age between 18-90 years old) attending the SMS Hospital were recruited to participate in this study. Fifty patients with isolated hypertension (42 males, mean age 54.16 ± 8.4 years) and 50 age matched healthy subjects (42 males, mean age 52.17 ± 8.6 years) were studied. Exclusion criteria were: secondary hypertension, angina pectoris, previous myocardial infarction, heart valve disease, HF, atrial fibrillation, chronic obstructive pulmonary disease, diabetes mellitus, and poor image quality on echocardiography.
All subjects underwent a routine physical examination, including body surface area (BSA) calculation using Du Bois and Du Bois formula, followed by a standard transthoracic echocardiogram (TTE). Before TTE, blood pressure was measured using a conventional sphygmomanometer, with the patient in supine position. Three measurements obtained at 5-minute intervals, were averaged. Hypertension was diagnosed in the presence of increased systolic BP (BPs) ≥140 mmHg and/or diastolic BP (BPd) ≥90 mmHg on two consecutive clinic visits and/or if patients were treated with antihypertensive drugs. 29,30
The age-matched control group included normo-tensive healthy subjects free from cardiovascular risk factors.
The protocol was approved by the local research Ethics Committee and a written informed consent was obtained from each subject.
Echocardiography:
Conventional Measurements:
Two-dimensional (2D) grayscale harmonic images were obtained in the left lateral position using a commercially available ultrasound system (i-33 PHILIPS) equipped with a cardiac M4S transducer. All measurements were averaged from three heart beats. LV wall thickness, diameters, volumes and EF were measured according to the American Society of echocardiography (ASE) recommendations.31, 32 The end-diastolic relative wall thickness (RWT) was also calculated, and a cut-off value of ≥0.45 was taken into account to define a concentric remodeling.31
The LV mass was determined with the area-length method,(31) and the LV mass index was calculated as ratio LV mass/BSA (g/m²).The diagnosis of LV hypertrophy was based on a LV mass index (LVMI) >102 g/m² in men and >81 g/m² in women.(32) Hypertensive patients were divided in two subgroups: subjects without LV hypertrophy (LVH(–)) ,and subjects with LV hypertrophy (LVH(+)).
Global Longitudinal Function by TDI:
Color TDI cineloops of three cardiac cycles from both four- and two-chamber views, obtained at end-expiratory apnea, were acquired and digitally stored. Gains were minimized to have a clear tissue signal with minimal background noise. To acquire the highest tissue velocities, the angle between the Doppler beam and mitral annulus was adjusted to a minimal level (<20º). From stored color TDI loops, a PW Doppler sample was set, offline, at the level of the septal and lateral corner (apical four-chamber view), and anterior and inferior corner (apical two-chamber view) of mitral annulus. The peak of systolic (S’), early diastolic velocity (E’) and late diastolic velocity (A’) was calculated for each corner. The results were averaged to obtain a mean value of S’, E’ and A’.
Global Strains by Speckle Tracking Echocardiography.
The 2D images acquired in the short and long axis planes analyzed using the custom acoustic-tracking software that allows a semi-automated analysis of ventricular dynamics (Q-lab PHILIPS INC.)
For LV strain (longitudinal (LS), circumferential (CS), and radial (RS)) evaluation, both apical (four-, two-, and three-chamber), and para-sternal short-axis (at mid papillary level) views obtained.Three consecutive end-expiratory cycles, in grayscale (frame rate = 60 to 80 frames/s) stored for each view and subsequently transferred to an Q-LAB workstation
The analysis of 2D strain was performed offline, using a semiautomatic tracking of LV. After manually tracking the endocardial border on a 2D image end-systolic frame, the software automatically tracked myocardial motion, creating six equidistant speckle tracking regions of interest for each image. Global LS, CS, and RS were obtained by calculating the average strain derived by myocardial tracking from each view
Statistical Analysis:
Data were expressed as mean ± SD. Statistical analysis was performed using the SPSS statistical software (SPSS v.17 for Windows, SPSS Inc., Chicago, IL, USA). For any parameter, independent t-test and ANOVA were used to compare variables between different groups. The chi square test and Fisher’s exact test were used for categorical variables. Linear regression analysis, with Pearson’s coefficient, was used to estimate correlation between continuous variables. P values ≤ 0.05 were considered significant
Results:
Population
All subjects were in sinus rhythm without signs and/or symptoms of HF (NYHA class I; Table 1). No difference between patients and controls was observed regarding: age, gender and heart rate (P = ns).34 %of hypertensive subject had evidence of concentric remodeling. As expected, most controls had normal LV mass index and geometry. No difference between LVH(–) and LVH (+) patients was found with respect to systolic (152.3±8.89 mmHg vs. 157.2±7.38 mmHg, P = ns) and diastolic blood pressure (97.36±7.27 mmHg vs. 99.24±6.74 mmHg,P = ns).
Table 1. Demographic and Clinical Data of All Subjects| Controls(n=50) | LVH(–) (n = 33) | LVH(+) (n = 17) | *P | **P | #P | |
| Age (Yr) | 52.26±8.61 | 54.73±8.05 | 53.71±9.46 | 0.075 | 0.078 | 0.691 |
| Gender (M/F) | 42/08 | 28/05 | 14/03 | - | - | - |
| HR(beats/min) | 70±13.2 | 68.8±9.2 | 66.6±9.7 | ns | ns | ns |
| Systolic BP (mmHg) | 123.8±7.76 | 152.3±8.89 | 157.2±7.38 | <0.0001 | <0.0001 | 0.054 |
| Diastolic BP (mmHg) | 78.2 ±2.75 | 97.36±7.27 | 99.24±6.74 | <0.0001 | <0.0001 | 0.382 |
LV Function by Conventional Echocardiography:
LVEF was normal both in LVH(–) and in LVH(+) patients; LV wall thickness, RWT were significantly increased in both LVH(–) and LVH(+) patients with respect to controls. As expected, thickness, RWT and LVMI were significantly higher in LVH (+) than in LVH(–) patients (P < 0.001). The RWT in the LVH(+) group was 0.47 ± 0.09%, as an expression of concentric hypertrophy. (Table 2)
Table 2. Conventional Echocardiographic FindingsTDI and Speckle Tracking Analysis:
Analysis of LV systolic and diastolic function by means of TDI showed different findings according to the LV geometry pattern (Table 3). In the LVH(–) patients (normal geometry), S’ and E’ velocities, as well as the A’ were normal, without any significant difference with respect to controls (S’ = 9.29 ± 0.98 cm/s vs. 9.64 ± 1.05 cm/s,P = ns; E’ = 11.03 ±3.06cm/s vs. 11.24 ±1.73 cm/s,P = ns; A’ 7.03 ± 2.95 vs. 6. 73 ± 1.41, P = ns);whereas in the LVH(+) group (concentric hypertrophy) S’ and E’ velocity were decreased and A’ velocity was increased in comparison to controls (S’ = 7.29± 0.58 cm/s vs. 9.64 ± 1.05 cm/s,P < 0.001; E’ = 6.55 ± 1.45 cm/s vs 11.24 ±1.73cm/s, P < 0.001, A’ = 10.24± 1.88 vs. 6. 73 ± 1.41,P < 0.001).
Table 3. TDI and STE Results| Controls(n=50) | LVH(–) (n = 33) | LVH(+) (n = 17) | *P | **P | #P | |
| S' | 9.64±1.05 | 9.29±0.98 | 7.29±0.58 | 0.06 | <0.0001 | <0.0001 |
| E' | 11.24±1.73 | 11.03±3.06 | 6.55±1.45 | 0.17 | <0.0001 | 0.003 |
| A' | 6.73±1.41 | 7.03±2.95 | 10.24±1.86 | 0.32 | <0.0001 | 0.133 |
| LS %(-) | 19.31±1.87 | 16.3±2.01 | 12.91 ±1.67 | <0.0001 | <0.0001 | <0.0001 |
| CS %(-) | 18.98±1.56 | 17.31±2.28 | 14.62 ±1.21 | <0.0001 | <0.0001 | <0.0001 |
| RS %(+) | 18.88±1.54 | 19.22±1.90 | 20.38 ±2.08 | 0.380 | 0.003 | 0.054 |
On the other hand, STE revealed relevant changes in LV mechanics even in patients with normal geometry (LVH(–)): these subjects, characterized by normal LV function on TDI, had an impaired systolic LS (–16.3±2.01 % vs. –19.31±1.87 %, P = <0.0001) and CS (–17.31±2.28 % vs. –18.98±1.56 %, P = <0.0001), with normal RS (19.22±1.90 % vs. 18.88±1.54 %, P = 0.38) when compared to healthy subjects (Figure 1). Moreover, in the LVH(+) patients STE revealed lower LS (–12.91 ±1.67 % vs. – 19.31±1.87 ,CS -14.62 ±1.216%, vs -18.98±1.56 P<0.001, Figure 1) and higher RS (20.38±1.56 % vs. 18.88±1.54 %, P = 0.003), (Figure 1).
Figure 1.Global longitudinal strain (panel A), circumferential strain (panel B), and radial strain (panel C) by STE in controls, LVH(–) and LVH(+) patients A. Longitudinal strain is lower both in LVH(–) (P =< 0.0001) and even more in LVH(+) patients (P < 0.0001), compared to controls; furthermore, it is lower in LVH(+) than in LVH(–) group (P = <0.0001). B. Circumferential strain is lower both in LVH(–) (P = <0.0001) and LVH(+) patients (P = <0.0001), in comparison with controls, and it is significantly decreased (P =< 0.0001) in LVH(+) than in LVH(–) patients. C. Radial strain is normal in LVH(–) (P = ns) and higher in LVH(+) patients (P = 0.003), in comparison with controls, and it is insignificantly higher (P = 0.05) in LVH(+) than in LVH(–) group. All these findings suggest that progressive adaptative changes occur in LV mechanics from patients with normal geometry to those with concentric hypertrophy.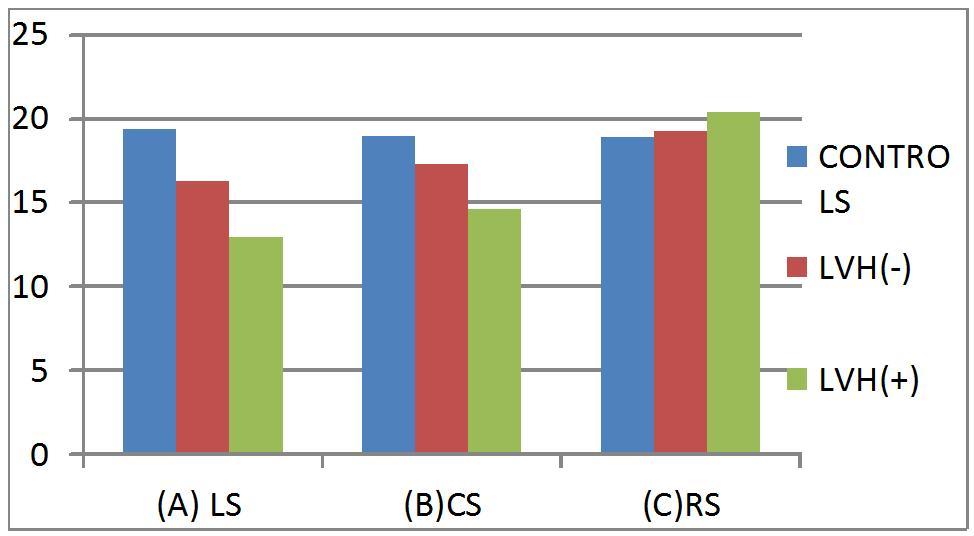
Pearson’s Linear Correlations:
The following relationships have been observed:
(1) Systolic blood pressure was inversely related with LS (r = –0.73, P < 0.0001); CS (r = –0.61, P < 0.0001); and positively with RS (r = 0.22, P =0.02). (2) The systolic blood pressure was also inversely related with S’ (r = –0.75, P < 0.0001); E’ (r = –0.65, P < 0.0001); and positively related with A’ (r = 0.55, P < 0.0001).Similar correlation were found with diastotic blood pressure.(3) In hypertensives we found a significant inverse relation between LV mass and indices of global LV systolic function, including both LS (r = –0.1; p<0.001) and CS ( r = – 0.59; p<0.0001)
Discussion:
Hypertensive patients without symptoms and/or signs of HF and with normal contractile function, as explored with conventional echocardiography, show subtle adaptative changes of LV systolic mechanics, which can be identified only by Speckle Tracking Echocardiography. This technique permits the detection of early LV diastolic function changes in hypertension,33 and also reveals that, in hypertensive patients free from clinical manifestations of HF, the earliest myocardial impairment involves the longitudinal fibers.34
The main findings of this research are:
(1) Hypertension results in early changes of LV mechanics that begin even before LV hypertrophy occurs, as suggested by 2D LS and CS reduction in patients with normal LV geometry (Stage A).
(2) In hypertension, alterations in LS and CS, as well as RS changes are related to LV concentric hypertrophy (Stage B).
LV Mechanics in Patients with Normal Geometry (Stage A):
It is well known, and confirmed by this study, that a preclinical systolic dysfunction occurs in hypertensive patients with LV hypertrophy.35, 36
We have observed, in addition, an impairment of longitudinal and circumferential systolic function even in patients with normal LV geometry. In this respect, STE appears more sensitive than both conventional echocardiography and TDI in identifying a reduction of intrinsic myocardial contractility, evident in hypertensive patients even long before LV hypertrophy becomes detectable. This finding highlights the advantages of 2D strain over TDI in early identifying LV systolic function impairment.
These early changes of myocardial contractility may be secondary to hemodynamic and/or biochemical alterations. The increased end-systolic wall stress, an expression of afterload, as well as the loading conditions, are likely to play a role in determining the longitudinal dysfunction in HHD. On the other hand, the chronic increase of endsystolic wall stress may promote subendocardial synthesis of collagen, thereby contributing to reduction of longitudinal deformation. With regard to the biochemical changes, myocardial fibrosis is one of the factors responsible for myocardial function deterioration in hypertension 37,38 in affected patients with normal EF, impaired LS and increased LV torsion are directly related with serum levels of tissue inhibitor of metalloproteinase-1 matrix, a marker of myocardial fibrosis.39 This suggests that abnormal collagen turnover and myocardial fibrosis may contribute to early LV contractile dysfunction.40, 41 On the other hand, in this study we observed that RS is preserved in hypertensive patients without structural LV changes.
LV Mechanics in Patients with Concentric Hypertrophy (Stage B):
LV hypertrophy is a common response to increased and prolonged afterload and is an independent predictor of cardiovascular morbidity and mortality.42, 43, 44, 45, 46 LV hypertrophy is associated with a variety of alterations including: fibrosis, impaired coronary artery vasodilatory capacity, depressed LV wall mechanics, and abnormal LV diastolic filling pattern.47, 48, 49, 50, 51 Subendocardium is susceptible to the deleterious effects of both interstitial fibrosis and hypoperfusion, to the extent that in HHD impairment of the subendocardial function results in abnormal longitudinal function.52 This is also suggested by a recent study based on 3D wall motion tracking analysis, demonstrating that myocardial strain pattern depends on LV adaptative responses to high blood pressure.53 Our results show that in a relatively late stage of HHD, corresponding to stage B of HF, additional LV changes occur, such as increase of RS, suggesting an involvement of mid-myocardial layers. The finding is consistent with the results of a recent study, demonstrating that in hypertension LV longitudinal systolic function progressively deteriorates.54
Limitations:
A limitation of this study is the small size of the sample; this is dependent on the inclusion of highly selected hypertensive patients (without additional cardiovascular risk factors and/or history of angina and/or myocardial infarction and/or heart valve disease, etc.), with exclusion of those with poor acoustic window. A further limitation is that we have included for the assessment of LV mechanics patients treated with antihypertensive drugs
Conclusions:
Speckle tracking echocardiography reveals LV mechanics alterations in hypertensive patients in a very early phase of the disease (Stage A of
ACC/AHA classification of HF) and provides new information on the pathophysiology of myocardial response to hypertension
References
- 1.Levy D, Larson M G, Vasan R S. (1996) The progression from hypertension to congestive heart failure.JAMA; 275:. 1557-1562.
- 2.Burt V L, Whelton P, Roccella E J.. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988–1991. Hypertension 1995;25: 305-313.
- 4.Sadler D B, Aurigemma G P, Williams D W. (1997) Systolic function in hypertensive men with concentric remodeling. , Hypertension; 30, 777-781.
- 5.G de Simone, Devereux R B, Celentano A. (1999) Left ventricular chamber and wall mechanics in the presence of concentric geometry. , J Hypertens; 17, 1001-1006.
- 6.Rusconi C, Sabbini T, Faggiano P. (2001) Prevalence of isolated left ventricular diastolic dysfunction in hypertension as assessed by combined transmitral and pulmonary venous Doppler flow. , Am J Cardiol; 87, 357-360.
- 7.Wachtell K, Smith G, Gerdts E. (2000) Left ventricular filling patterns in patients with systemic hypertension and left ventricular hypertrophy (the life study). , Am J Cardiol; 85, 466-472.
- 8.Banerjee P, Banerjee T, Khand A. (2002) et al: Diastolic heart failure: Neglected or misdiagnosed?. , J Am Coll Cardiol 39, 138-141.
- 9.Garcia E H, Perna E R, Farias E F. (2006) Reduced systolic performance by tissue Doppler in patients with preserved and abnormal ejection fraction: New insights in chronic heart failure. , Int J Cardiol; 108, 181-188.
- 10.Sanderson J, Fraser A. (2006) Systolic dysfunction in heart failure with a normal ejection fraction: Echo-Doppler measurements. Prog Cardiovasc Dis;. 49, 196-206.
- 12.Vinereanu D, Nicolaides E, Tweddel A C. (2005) Pure” diastolic dysfunction is associated with long-axis systolic dysfunction: Implications for the diagnosis and classification of heart failure. , Eur J Heart Fail; 7, 820-828.
- 13.Yip G, Zhang Y, Tan P. (2002) Left ventricular long-axis changes in early diastole and systole: Impact of systolic function on diastole. , Clin Sci (Lond); 102, 515-522.
- 14.Yip G, Wang M, Zhang Y. (2002) Left ventricular long axis function in diastolic heart failure is reduced in both diastole and systole: Time for a redefinition?. , Heart; 87, 121-125.
- 15.Yu C, Lin H, Yang H.et al: Progression of systolic abnormalities in patients with “isolated” diastolic heart failure and diastolic dysfunction. Circulation 2002;105:. 1195-1201.
- 16.Aurigemma G, Silver K, Priest M. (1995) Geometric changes allow normal ejection fraction despite depressed myocardial shortening in hypertensive left ventricular hypertrophy. , J Am Coll Cardiol; 26, 195-202.
- 17.Ballo P, Quatrini I, Giacomin E. (2007) Circumferential versus longitudinal systolic function in patients with hypertension: A non linear relation. , J Am Soc Echocardiogr; 20, 298-306.
- 18.Palmon L, Reichek N, Yeon S, et.al: Intramural myocardial shortening in hypertensive left ventricular hypertrophy with normal pump function. Circulation 1994;89:. 122-131.
- 19.Yuda S, Short L, Leano R. (2002) Myocardial abnormalities in hypertensive patients with normal and abnormal left ventricular filling: A study of ultrasound tissue characterization and strain. , Clin Sci; 103, 283-293.
- 20.Poulsen S, Andersen N H, Ivarsen P I, et.al: Doppler tissue imaging reveals systolic dysfunction in patients with hypertension and apparent ‘isolated’ diastolic dysfunction. , J Am Soc Echocardiogr; 16, 724-731.
- 21.Aurigemma G P, Silver K H, Priest M A, Gaasch W H. (1995) Geometric changes allow for normal ejection fraction despite depressed myocardial shortening in hypertensive left ventricular hypertrophy. , J Am Coll Cardiol; 26, 195-202.
- 22.G de Simone, Devereux R B, Koren M J, Mensah G A, Casale P N et al. (1996) Midwall left ventricular mechanics. An independent predictor of cardiovascular risk in arterial hypertension. , Circulation; 93, 259-265.
- 23.Hurlburt H M, Aurigemma G P, Hill J C, Narayanan A, Gaasch W H et al. (2007) Direct ultrasound measurement of longitudinal, circumferential and radial strain using 2-dimensional strain imaging in normal adults. , Echocardiography; 24, 723-731.
- 24.Amundsen B H, Helle-Valle T, Edvardsen T. (2006) Noninvasive myocardial strain measurement by speckle tracking echocardiography: Validation against sonomicrometry and tagged magnetic resonance imaging. , J Am Coll Cardiol; 47, 789-793.
- 25.Reisner S A, Lysyansky P, Agmon Y. (2004) Global longitudinal strain: A novel index of left ventricular systolic function. , J Am Soc Echocardiogr; 17, 630-633.
- 26.Hurlburt H M, Aurigemma G P, Hill J C, et.al: Direct Ultrasound Measurement of Longitudinal, Circumferential, and Radial Strain Using 2-Dimensional Strain Imaging in Normal Adults. Echocardiography 2007;24:. 723-731.
- 27.Van Dalen BM, Soliman O, Vletter W B. (2009) Insights into Left Ventricular Function from the Time Course of Regional and Global Rotation by Speckle Tracking Echocardiography. , Echocardiography; 26, 371-377.
- 28.Hunt S A, Abraham W T, Chin M H. (2009) . Focused Update Incorporated Into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults J Am Coll Cardio 2009;14:e1–e90 .
- 30.Chobanian A V, Bakris G L, Black H R. (2003) . National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA 2003;289: 2560-2572.
- 31.Lang R M, Devereux RB BierigM. (2005) Chamber Quantification Writing Group; American Society of Echocardiography’s Guidelines Standards Committee European Association of Echocardiography Recommendations for chamber quantification: A report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. , J Am Soc Echocardiogr; 18, 1440-1463.
- 32.Schiller N B, Shah P M, Crawford M, et. (1989) al: Recommendations for quantitation of the left ventricle by two dimensional echocardiography. , American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 2, 358-367.
- 33.Mu Y, Qin C, Wang C.Two-Dimensional Ultrasound Speckle Tracking Imaging in Evaluation of Early Changes in Left Ventricular Diastolic Function in Patients with Essential Hypertension. Echocardiography 2010;27:. 146-154.
- 34.Mizuguchi Y, Oishi Y, Miyoshi H. (2008) The functional role of longitudinal, circumferential, and radial myocardial deformation for regulating the early impairment of left ventricular contraction and relaxation in patients with cardiovascular risk factors: A study with two-dimensional strain imaging. , J Am Soc Echocardiogr; 21, 1138-1144.
- 35.Mizuguchi Y, Oishi Y, Miyoshi H, et. (2010) al: Concentric left ventricular hypertrophy brings deterioration of systolic longitudinal, circumferential, and radial myocardial deformation in hypertensive patients with preserved left ventricular pump function. , J Cardiol 55, 23-33.
- 36.Aurigemma GP Narayanan, Chinali M. (2009) et al: Cardiac Mechanics in Mild Hypertensive Heart Disease A Speckle-Strain Imaging Study. Circ Cardiovasc Imaging. 2, 382-390.
- 37.Komuro I, Katoh Y, Kaida T. (1991) Mechanical loading stimulates cell hypertrophy and specific gene expression in cultured rat cardiac myocytes. , J Biol Chem; 266, 1265-1268.
- 38.Brilla C G, Janicki J S, Weber.KT: Impaired diastolic function and coronary reserve in genetic hypertension: Role of interstitial fibrosis and medial thickening of intramyocardial coronary arteries. Circ Res 1991;69:. 107-115.
- 39.Martinez D A, Guhl D J, Stanley W C, Vailas A C. (2003) Extracellular matrix maturation in the left ventricle of normal and diabetic swine. , Diabetes Res Clin Pract; 59, 1-9.
- 40.Kang S J, Lim H S, Choi B J. (2008) Longitudinal strain and torsion assessed by two-dimensional speckle tracking correlate with the serum level of tissue inhibitor of matrix metalloproteinase-1, a marker of myocardial fibrosis, in patients with hypertension. , J Am Soc Echocardiogr 21, 907-911.
- 41.Sengupta P P, Narula J.Reclassifying heart failure: Predominantly subendocardial, subepicardial, and transmural. Heart Failure Clin 2008;4:. 379-382.
- 42.Casale P N, Devereux R B, Milner M. (1986) Value of echocardiographic measurement of left ventricular mass in predicting cardiovascular morbid events in hypertensive men. , Ann Intern Med; 105, 173-178.
- 43.Levy D, Garrison R J, Savage D D. (1990) Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. , N Engl J Med;322: 1561-1566.
- 44.Haider A W, Larson M G, Benjamin E J. (1998) Increased left ventricular mass and hypertrophy are associated with increased risk for sudden death. , J Am Coll Cardiol; 32, 1454-1459.
- 45.Koren M J, Devereux R B, Casale P N. (1991) Relation of left Ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. , Ann Intern Med; 114, 345-352.
- 46.Krumholz H M, Larson M, Levy D. (1995) Prognosis of left ventricular geometric patterns in the Framingham Heart Study. , J Am Coll Cardiol; 25, 879-884.
- 47.Weber K T, Brilla C G. (1991) Pathological hypertrophy and cardiac interstitium: Fibrosis and renin-angiotensinaldosterone system. , Circulation; 83, 1849-1865.
- 48.Querejeta R, Varo N, L´opez B. (2000) Serum carboxyterminal propeptide of procollagen type I is a marker of myocardial fibrosis in hypertensive heart disease. , Circulation; 101, 1729-1735.
- 49.Conrad C H, Brooks W W, Hayes J A. (1995) Myocardial fibrosis and stiffness with hypertrophy and heart failure in the spontaneously hypertensive rats. , Circulation; 91, 161-170.
- 50.Brilla C G, Janicki J S, Weber K T. (1991) Impaired diastolic function and coronary reserve in genetic hypertension: Role of interstitial fibrosis and medial thickening of intramyocardial coronary arteries. , Circ Res; 69, 107-115.
- 51.Martinez D A, Guhl D J, Stanley W C. (2003) Extracellular matrix maturation in the left ventricle of normal and diabetic swine. Diabetes Res Clin Pract;59:. 1-9.
- 52.Lumens J, Delhaas T, Arts T. (2006) Impaired subendocardial contractile myofiber function in asymptomatic aged humans, as detected using MRI. Am J Physiol Heart Circ Physiol;.
