Localization of Angina Related Artery by Admission ECG in Unstable Angina and NSTEMI Patients
Abstract
Objective:
To find out the diagnostic accuracy of admission ECG against coronary angiography (CAG) to predict the ARA in patients with USAP /NSTEMI.
Background:
In USAP even though multiple active plaques are documented, one critical lesion would be responsible for the index episode of angina. Contrary to STEMI there is no standard methodology to identify the Angina related artery (ARA) in USAP.Therefore we plan to determine whether admission ECG could predict the ARA in patients with USAP/NSTEMI.
Patients and Methods:
250 eligible patients with USAP/NSTEMI undergoing coronary angiography were enrolled in the study. After locating the ARA , the patient’s admission ECG was compared with CAG finding to study whether it has any predictive value for identifying ARA.
Results:
Sensitivity of the admission ECG for LAD as ARA was 73.6%, Specificity was 93.5%, PPV was 90%, NPV was 81.8%, +LR 10.4, Posterior probability 0.89, -LR 0.29, Posttest odds 0.22. Similarly for RCA and LCx ,Sensitivity was 63.1%, Specificity was 93.7%, PPV was 90.5%, NPV was 72.7%, +LR 9, Posterior Probability 0.89, -LR 0.35, Posttest odds 0.33. For the LM and TVD, Sensitivity was 66.6%, Specificity was 98.5%, PPV was 91.4%, and NPV was 92.5%, +LR 33, Posterior Probability 0.89, -LR 0.33, Posttest odds 0.08.
Conclusion:
With high +LR, Admission ECG is moderately sensitive and highly specific for detecting culprit artery.
Author Contributions
Academic Editor: Osmar Centurion, Professor of Medicine. Asuncion National University. Cardiology Division. First Department of Internal Medicine. Asuncion. Paraguay
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2016 Arpan P. Desai, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Unstable angina together with acute myocardial infarction and sudden cardiac death consist the acute coronary syndrome. Unstable angina and myocardial infarction without ST-segment elevation accounts for approximately 2 million to 2.5 million hospital admissions annually worldwide1.Several studies in the past years have described the angiographic morphology of coronary lesions in acute coronary syndromes2, 3, 4, 5, 6. Unstable angina( USAP /NSTEMI ) constitute a heterogeneous group of patients with lesions ranging from normal coronary artery to severe multi vessel disease. ST depression ( or transient ST elevation) and T wave changes occur in up to 50% of patients of USAP/NSTEMI 7.In unstable angina, eccentric, irregular, ulcerated lesions with possible presence of thrombus are more frequent. They are usually due to the fissuring or rupture of atherosclerotic plaque. In TACTICS- TIMI 18 trial, patients with USAP/NSTEMI have following findings on coronary angiography. 34% had Triple vessel disease (TVD) (>50% luminal diameter stenosis), 28% had Double vessel disease (DVD), 26% had single vessel disease (SVD), 13% had no significant stenosis, 10% had left main (LM) stenosis of >50%. Even though multiple active plaques are documented, one critical lesion would be responsible for the index episode of angina. Contrary to STEMI there is no standard methodology to identify the Angina related artery (ARA) in USAP. Therefore we plan to determine whether admission ECG could predict the ARA in patients with USAP/NSTEMI.
Aims & Objectives
1)To find out the diagnostic accuracy of admission ECG against coronary angiography (CAG) to predict the ARA in patients with USAP /NSTEMI.
Diagnostic accuracy in terms of sensitivity, specificity, Positive predictive value (PPV), Negative predictive value (NPV), Positive likely hood ratio(+LR), posterior probability, Negative likely hood ratio(-LR), post test odds.
2) To describe the profile of associated risk factors among USAP/ NSTEMI cases.
Methods
This hospital based observational descriptive study for the diagnostic accuracy of admission ECG for identification of ARA in USAP/NSTEMI patients against CAG was conducted at department of Cardiology, SMS hospital, Jaipur in between April 2012 to Feb 2013. Patients with Unstableangina were defined as having angina pectoris (or equivalent type of ischemic discomfort) with at least one of three features: (1) occurring at rest (or minimal exertion) and usually lasting >20 minutes (if not interrupted by the administration of a nitrate or an analgesic); (2) being severe and usually described as frank pain; or (3) occurring with a crescendo pattern (i.e., pain that awakens the patient from sleep or that is more severe, prolonged, or frequent than previously). Patients with unstable angina who had evidence of myocardial necrosis on the basis of elevated cardiac serum markers, such as cardiac-specific troponin T or I and creatine kinase isoenzyme (CK)–MB, were diagnosed as NSTEMI 8. Patients with post infarction angina, h/o CABG,h/o PCI, old MI, Inability or unwillingness to consent were excluded from the study. 250 eligible patients with the diagnosis of USAP/NSTEMI who met the inclusion criteria were considered for study. All patients were assessed by use of a structured questionnaire regarding main risk factors and medical history. All patients underwent a detailed examination, 12 lead surface ECG + High lateral and Right sided leads, and standard laboratory tests (CBC, LFT, RFT and Lipid profile), Transthorasic 2D echo done in all cases.
Cardiac Catheterization
All patients underwent diagnostic coronary angiography (CAG) either through the transfemoral or transradial route. All obstructive lesions were visualized in two orthogonal views and lesion with a visual diameter stenosis of 50% was considered significant9.CAG was done by the cardiologist other than investigator. Investigator had demarcated ECG finding before comparing it with CAG finding.
Determination of ECG Criteria
In absence of defined ECG criteria for localization of culprit artery in USAP/NSTEMI, the most common ECG pattern found in respective culprit artery diagnosed by Angiography was considered the criteria for ECG localization.
Culprit Lesion Determination
In each case we attempted to identify the ARA. Patients who have single vessel disease the ARA localization was straight forward 10. Patients who have multi vessel disease, the coronary lesion was considered angina related if the Regional Wall Motion Abnormality (RWMA) detected by echocardiography matched myocardial segments supplied by the arterial territory containing the lesion or if there is obvious eccentric thrombus with scalloped or overhanging edges and a narrow neck on CAG10. Features suggesting thrombus include globular intraluminal mass with rounded or polypoid shape, or ‘’Haziness’’ of a lesion. After locating the ARA , the patient’s admission ECG was compared with CAG finding to study whether it has any predictive value for identifying ARA. Similarly in case of multiple culprit arteries specific ECG pattern were compared against coronary angiography results.
Statistical Analysis
Quantitative data were summarized in form of mean & SD. Qualitative data were summarized in form of proportions. Diagnostic accuracy was analyzed by sensitivity, specificity, PPV and NPV. Positive and negative Likelihood ratios, posttest odds and posterior probabilities were also computed.
Results
Mean age of the study population was 56.79 ± 10.75yrs, 18.4 % (46) patients were female, and 34.4 % (86) patients had NSTEMI. 23.2 % (58) patients had DM, 39.2 % (98) patients had HT, 49.2 % (123) patients were smokers, and 32% (80) patients had dyslipidemia. Mean total cholesterol of the study cases was 272.4 ± 41.63 mg/dl, Mean LDL was 138.89±22.72 mg/dl, Mean HDL was 50.38 ± 7.55mg/dl, and Mean Triglyceride was 158 ± 35.3 mg/dl, 27.6 % (69) patients had positive family history of IHD 11.In present study in 41(16.4%) patients with Multivessel disease cases we were able to localize ARA with the help of 2D echo and in 25 cases, we were able to localize ARA with help of thrombus containing lesion. SVD with stenosis ≥50% was observed in 119 (47.6%) patients, DVD was observed in 60 (24%) patients, TVD in 38 (15%) and LM disease was observed in 15 (6%) patients. The culprit artery was the left anterior descending artery (LAD) in 61 (24.4%) patients, the Left circumflex artery (LCx) in 28 (11.2%), the right coronary artery (RCA) in 27 (10.8%), the Ramus intermedius in 3(1.2%). The LAD + RCA were culprit in 24(9.6%), the LAD + LCx in 25(10%), the RCA + LCx in 11(4.4%) patients. These 60 patients with DVD were considered independently in their respective lesion groups e.g. if a case had LAD and RCA both as culprit arteries as per angiography, then the case’s ECG findings were considered in both LAD as well as RCA group as per the respective ECG criteria. Angiography showed either normal or insignificant coronary artery disease In 28(11.2%) patients (shown in Figure 1). After locating the ARA, the patient’s admission ECG was compared with CAG finding to study whether it has any predictive value for identifying ARA. For LAD as a culprit artery the most common ECG pattern observed was ST depression and/ or T inversion in leads V1 to V5. Subsequently sensitivity, specificity, PPV, NPV, +LR, -LR, posttest odds and posterior probabilities were calculated for LAD as a culprit artery keeping the criteria of ST-segment depression of ≥ 0.05mv or T wave inversion of ≥ 0.3mv in leads V1 to V5.Sensitivity was 73.6%, Specificity was 93.5%, PPV was 90%, NPV was 81.8%, +LR 10.4, Posterior probability 0.89, -LR 0.29, Post test odds 0.22. For LCx (dominant) and RCA as a culprit artery, the most common ECG pattern observed was ST depression and/ or T inversion in leads II, III, aVf, V5, V6, and for Non dominant LCx were ST depression and/ or T inversion in leads II, III, avF.
Figure 1.Showing the Distribution of ARA in study cases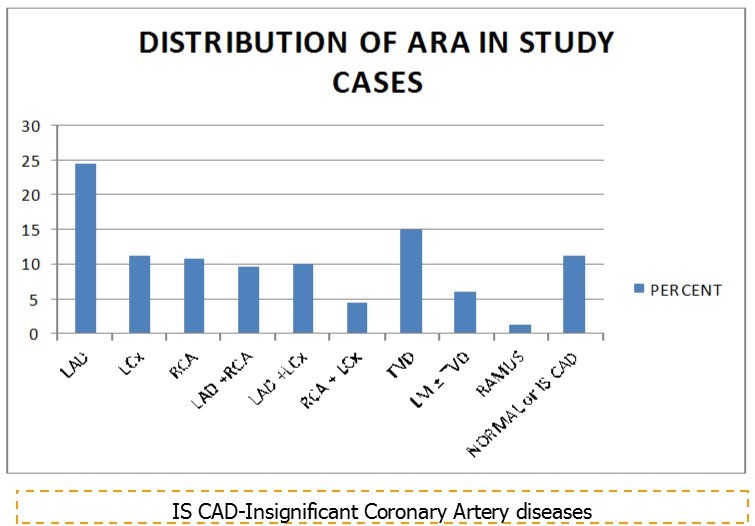
Sensitivity, specificity, PPV, NPV, +LR, Posterior Probability, -LR and Post test odds of the Admission ECG were calculated for LCx or RCA as a culprit artery keeping the criteria of ST-segment depression of ≥ 0.05mv or T wave inversion of ≥ 0.3mv in leads II, III, avF, V5, V6.Sensitivity was 63.1%, Specificity was 93.7%, PPV was 90.5%, NPV was 72.7%, +LR 9, Posterior Probability 0.89, -LR 0.35, Post test odds 0.33. For patients with Left Main and/ or triple vessel disease, the most common ECG pattern observed was ST elevation in lead avR with ST depression and/ or T inversion in other limb leads & precordial leads. The predictive value of ECG (with ≥0.05mm of ST elevation in lead avR with ST depression of ≥ 0.05mv and/ or T inversion of ≥ 0.3m in 8 other limb leads & precordial leads) for LM and or TVD in the form of Sensitivity was 66.6%, Specificity was 98.5%, PPV was 91.4%, and NPV was 92.5%, +LR 33, Posterior Probability 0.89, -LR 0.33, Post test odds 0.08.
Discussion
In the present study mean age of the patients was around 7 years younger than the that of the western study10 ( 57.12 years as compare to 64 years respectively), more male (82% vs 66%), smoking much more prevalent (49.2% vs 24%). These data goes with the fact that in India Acute Coronary Syndrome (ACS) occurs at around one decade earlier, more prevalent in males, smoking is much more prevalent and leading cause of IHD.
In the present study SVD was more common than that found in TACTICS- TIMI 18 trial (47.6% vs 26%). Reason for this difference may be explained by the detection of ARA among Multivessel disease cases with the use of 2D echo and thrombotic lesion, which was not used in TACTICS- TIMI 18 trial. In present study thrombotic lesion was present in 10% cases. This is similar to previous study figure of 12% 13.
Unlike in case of STEMI, no similar study on the utility of admission ECG for localization of ARA was done in the past in case of USAP/NSTEMI patients. If the admission ECG is positive for LAD, it suggests LAD as culprit artery accurately in 73.6% cases. While if these changes are absent, ECG could rule out LAD as culprit artery accurately in 93.5% cases. When used with a pre-test probability of 0.44 (44%), ECG increases the probability of LAD as a culprit artery from 44% to 89% (Posterior probability of 0.89) when it is positive for LAD and it increases the probability of LAD not culprit artery from 56% to 81% when negative. Post test odds of 0.22 suggests that if patient has negative ECG pattern for LAD as culprit artery even then there are 22% chance that patient has LAD as culprit artery on CAG.
Similarly with the above mentioned criteria for RCA and LCx, ECG could suggest culprit artery accurately in 63.1% cases and in the absence of these changes ECG could rule out accurately in 93.7% cases. ECG when used with pre-test probability of 0.48 (48%), it increases the probability of RCA or LCx as a culprit artery from 48% to 89% (Posterior probability of 0.89) when it is positive for RCA or LCX and increases the probability of not culprit artery from 52% to 73% when negative. Post test odds of 0.33 suggests that if patient has negative ECG pattern for RCA or LCx as culprit artery even then there are 33% chance that patient has RCA or LCx as culprit artery on CAG.
For LM and TVD with the above mention criteria ECG could suggest culprit artery accurately in 66.6% cases, and absence of these changes ECG could rule out accurately in 98.5% cases. When used with a pre-test probability of 0.21 (21%), it increases the probability of LM or TVD as culprit artery from 21% to 89% (Posterior probability of 0.89) when it is positive for LM or TVD and it increases the probability of not culprit artery from 81% to 92% when negative. Post test odds of 0.08 suggests that if patient has negative ECG pattern for LM or TVD as culprit artery even then there are 8% chance that patient has LM or TVD as culprit artery on CAG. In AHA/ACCF/HRS Recommendation for standardization and interpretation of ECG, it has been found that in USAP patients with ST-segment depression in 8 or more body surface ECG leads, combined with ST elevation in avR, and is associated with a 75% predictive accuracy of LM or TVD stenosis 12. While in present study the predictive accuracy for LM or TVD was 92%.
The moderate sensitivity of ECG for localization of culprit arteries in present study (ranged from 63% to 73%) is explained by the facts that there are Individual variation in coronary anatomy and presence of Collateral circulation, LBBB, Preexcitation Syndrome, Left ventricular hypertrophy, Inadequate representation of posterior wall.
Limitations
We have considered the visual estimation method for percentage stenosis in our study that may incorporate subjective bias. Use of quantitative coronary angiography and IVUS could have been more objective and more informative for plaque morphology, complexity respectively.
We had taken only the most frequent pattern of ECG for calculation of sensitivity, specificity, PPV, NPV, so that the other ECG pattern are not taken into consideration.
Conclusions
Admission ECG is moderately sensitive and highly specific for detecting LAD as a culprit artery. When admission ECG is used, it increases the probability of LAD as a culprit artery from baseline pre-test value of 44% to 89% when positive for LAD and it increases the probability of LAD not culprit artery from 56% to 81% when negative. ECG is moderately sensitive and highly specific for detecting RCA or LCx as a culprit artery. When used with pre-test probability of 48%, it increases the probability of RCA or LCx as a culprit artery from 48% to 89% when positive for RCA or LCx, and increases the probability of not culprit artery from 52% to 73% when negative. ECG is fairly sensitive and highly specific for detecting LM or TVD as culprit artery. When used with a pre-test probability of 21%, it increases the probability of LM or TVD as culprit artery from 21% to 88% when positive for LM or TVD and it increases the probability of not culprit artery from 81% to 92% when negative.
Recommendation
With the moderate sensitivity, high specificity and high positive LR of admission ECG for localization of culprit artery, the utility of admission ECG needs further evaluation in USAP/NSTEMI cases. It would facilitate Physicians to focus on the intervention of the culprit artery like STEMI cases, consequently reducing the number of stent implantation and consequence associated with it.
Supplementary Material
Supplementry Figure 1.Bar diagram showing Diagnostic accuracy (in form of sensitivity, specificity, PPV and NPV) of Admission ECG for culprit artery localization
| Culprit artery | ECG criteria | Diagnostic Accuracy | |||||||||
| Sens | Spec | PPV | NPV | +LR | Post Pro | -LR | Post t odds | -LR | Post t odds | ||
| LAD | ST-segment depression of ≥ 0.05mv or T wave inversion of ≥ 0.3mv in leads V1 to V5 | 73.60% | 93.50% | 90% | 81.80% | 10.4 | 0.89 | 0.29 | 0.22 | 0.29 | 0.22 |
| RCA or LCx | ST-segment depression of ≥ 0.05mv or T wave inversion of ≥ 0.3mv in leads II, III, avF, V5, V6.(for non dominant LCx above changes in leads II, III, avF) | 63.10% | 93.70% | 90.50% | 72.70% | 9 | 0.89 | 0.35 | 0.33 | 0.35 | 0.33 |
| LM or TVD | ≥0.05mm of ST elevation in lead avR with or without ST depression of ≥ 0.05mv and/ or T inversion of ≥ 0.3m in 8 other limb leads & precordial leads | 66.60% | 98.50% | 91.40% | 92.50% | 33 | 0.89 | 0.33 | 0.08 | 0.33 | 0.07 |
References
- 1.Braunwald E, Antman E M, Beasley J W.ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: a report of the. , American College of Cardiology/ American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients with Unstable Angina). J Am Coll Cardiol 2000, 970-2.
- 2.Levin D C. (1982) Fallon JT: Significance of the angiographic morphology of localized coronary stenosis. Histopathologic correlations. Circulation. 66, 316-320.
- 3.Ambrose J A, Winters S L, Stern A, Eng A, Teichholz L E et al. (1985) Angiographic morphology and the pathogenesis of unstable angina pectoris. , J Am Coll Cardiol 5, 609-616.
- 4.Ambrose J A, Winters S L, Arora R R, Eng A, Riccio A et al. (1986) V: Angiographic evolution of coronary artery morphology in unstable angina. , J Am Coll Cardiol 7, 472-478.
- 5.Ambrose J A, Hjemdahl-Monsen C E, Borrico S, Gorlin R, Fuster V. (1988) Angiographic demonstration of a common link between unstable angina pectoris and non-Q wave acute myocardial infarction. , Am J Cardiol 61-244.
- 6.Ambrose J A. (1992) Plaque disruption and the acute coronary syndromes of unstable angina and myocardial infarction: if the substrate is similar, why is the clinical presentation different?. , J Am Coll Cardiol 19, 1653-1658.
- 7.Cannon C P, McCabe C H, Stone P H, et. (1997) al: The electrocardiogram predicts one-year outcome of patients with unstable angina and non–Q wave myocardial infarction:. , Results of the TIMI III Registry ECG Ancillary Study. J Am Coll Cardiol 30, 133.
- 9.Eugen Braunwald Weintraub. (2001) . TACTICS–THROMBOLYSIS IN MYOCARDIAL I NFARCTION 18.NEJM VOLUME 344JUNE21 .
- 10.Dangas Geogrge, Mehran Roxana. (1997) . Correlation of Angiographic Morphology and Clinical Presentation in Unstable Angina JACC 29, 519-25.
- 11.Maren T Scheuner, MPH William C Whitworth. (2006) MPHet al: Definition of a positive family history for coronary heart disease. Genet Med. 8(8), 491-501.
Cited by (6)
This article has been cited by 6 scholarly works according to:
Citing Articles:
V. Raju - Cureus (2023) Semantic Scholar
Cureus (2023) Crossref
Cureus (2023) OpenAlex
Rauf Shadab, Kumar Tarun, Kumar Vijay, Nath Ranjit Kumar - Journal of Cardiology and Cardiovascular Medicine (2023) Semantic Scholar
Journal of Cardiology and Cardiovascular Medicine (2023) Crossref
Journal of Cardiology and Cardiovascular Medicine (2023) OpenAlex
I. Ebeid, W. Farid, Ashraf Ahmed, N. Samy - (2020) Semantic Scholar
Cardiology and Cardiovascular Research (2020) OpenAlex
