Comment on the Stages of HIV Care Continuum: Considering Treatment for Secondary Prevention among Patients ‘Retained in Care’
Abstract
This commentary argues for incorporating secondary prevention into the HIV care continuum for patients retained in care. It outlines opportunities to reduce transmission through viral suppression, risk reduction counseling, and supportive services within routine visits.
Author Contributions
Copyright © 2014 H. Elsa Larson, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Letter to the Editor
In July 2012, the Centers for Disease Control (CDC) presented new data at the XIX International AIDS Conference indicating only 25% of Americans with HIV had a suppressed viral load.1 Viral suppression has been associated with reduced individual morbidity and mortality as well as reduced risk of transmission to sexual partners. The CDC study further reported on the proportion of Americans in each Stage of HIV Care: 1) testing and diagnosis, 2) linkage to care, 3) retention in care, 4) provision of antiretroviral therapy (ART), and 5) viral suppression. Their findings suggested that of all people living with HIV in the United States, 82% had been diagnosed, 66% had been linked to care, 37% were retained in care, 33% were prescribed antiretroviral therapy (ART), and 25% had achieved viral suppression. These Stages of Care results are consistent with previous estimates2, 3that suggest many HIV-infected individuals drop-off as they progress through the continuum, leaving only a minority of individuals who reach the final stage of viral suppression.
The Stages of Care continuum was first described by Gardner et al3 (March 2011) and is currently being used by federal, state, and local agencies to quantify the engagement of HIV-infected individuals in each stage of care and target resources accordingly. Achievement of viral suppression by adherence to ART is the model’s primary outcome for all people with HIV, and thus the model is alternatively referred to as the “treatment cascade.” The rationale for viral suppression as the cascade’s outcome is sound: 1) viral suppression is an expected result of adherence to ART, 2) viral suppression benefits the individual through improved clinical outcomes, and 3) viral suppression provides the public health benefit of reduced risk of transmission to others.
Treatment guidelines were updated in March 2012 to recommend initiation of ART in all HIV-infected patients,4 but this does not mean all patients will receive ART. Patients may refuse or postpone treatment, and providers may opt to defer therapy on a case-by-case basis. For example, the strength of the recommendation for early initiation varies by patient CD4 count as there is limited evidence to demonstrate a clear clinical risk-benefit ratio for asymptomatic patients with CD4 counts over 500. However, there is strong evidence to support the use of early ART to prevent sexual transmission of HIV. Results from the HPTN 052 trial demonstrated a 96% reduction in heterosexual transmission associated with early ART.5 Based on these and other data, early initiation of ART is now recommended for all patients who are at-risk of transmitting to sexual partners (regardless of CD4 count) for public health benefit. Providers’ decisions to treat an individual should consider the clinical benefits and limitations of early ART for each patient, while also evaluating the degree of transmission risk to partners and relative benefit of treatment to prevent secondary transmission.
Recently, we were interested in determining if HIV-infected patients with transmission risk6 (plasma viral loads ≥3500 and not currently on ART) received secondary prevention counseling from their providers. Based on an earlier study, it was estimated that 7-11% of these clinic patients may be at high biological risk for HIV transmission based on a higher plasma viral load and ART non-use.7 In October 2010, we conducted a retrospective cohort study using chart review and found that 6% of our clinic population (N=79) were at significant biological risk for transmission based on their plasma viral load.8 These cases were then dichotomized to the High-Risk (n=53) or Low-Risk (n=26) group based on behavioral risk. High-Risk was defined as ≥1 reported episode of unprotected vaginal or anal sex with an uninfected partner, ≥1 reported episode of needle-sharing with an uninfected partner, or ≥1 positive sexually transmitted infection result in the past 22 months. Low-Risk was defined as no reported sexual contact or needle-sharing with uninfected partners, only reported sex or needle-sharing with other HIV-infected partners, or 100% reported condom use. We found that 67% of these patients were categorized as High-Risk. Given the high behavioral risk of transmission within this group of patients with detectable plasma viral loads (≥3500), we explored factors to explain why these patients were not prescribed ART to decrease their risk of secondary transmission.* A post-hoc analysis of this group explained that 19% of these cases were noted to have adherence concerns (e.g. record of poor adherence, patient refusal, or noted clinical factor that might interfere with adherence). An additional 19% had been diagnosed within the previous six months, and we presumed that treatment may have been under consideration. The remaining 62% of cases in this group were defined as having ‘unexplained ART non-use.’ Among these cases, 61% had CD4 counts of >500, 33% were in the range of 350-500, and 6% were <350. It was concluded that the most likely hypothesis to explain deferred initiation of ART was physician adherence to 2010 treatment guidelines that recommended therapy for all asymptomatic patients with a CD4 cell count ≤500.9 As of March 2012, all patients known to be at risk for transmission are recommended candidates for early initiation of ART for secondary prevention, even if they are asymptomatic. The third boxed recommendation states that “effective ART also has been shown to prevent transmission of HIV from an infected individual to a sexual partner; therefore, ART should be offered to patients who are at risk of transmitting HIV to sexual partners (AI {heterosexuals} or AIII {other transmission risk groups})” 4. Prioritizing treatment for individuals to reduce risk of transmission to their partners can help achieve the goal of viral suppression for all. Our data described a group of patients engaged in care, not on ART, and at high-risk for transmitting HIV to their partners. These data, combined with recent estimates about viral suppression, suggest there may be utility to integrating tailored risk assessments into the treatment cascade. Clinical tools, models, or practices to better identify patients at-risk of transmission can accommodate treatment for secondary prevention purposes while synergistically facilitating stage progression from the “retained in care” stage to the “initiation of ART” stage. We propose a simple screening algorithm to stratify patients into risk categories based on their combined biological and behavioral risk profile. Our model, the ACT-R FACT-R (Algorithm to Categorize Transmission Risk) is a 3-tier algorithm to stratify patients to one of three categories: 1) At-Risk:no current biological or behavioral risk factors, 2) Higher Risk: behavioral or biological risk factor, or 3) Highest Risk: behavioral and biological risk factors (Figure 1). The results obtained from this brief screening could help providers identify patients likely to be core transmitters of HIV, and offer them ART and other recommended interventions10 that are matched to their current biological and behavioral risk profile (e.g. STI screening and treatment, brief behavioral interventions, risk reduction counseling, assessment for ART readiness and adherence concerns).
Figure 1.ACT-R FACT-R: Algorithm to Categorize Transmission Risk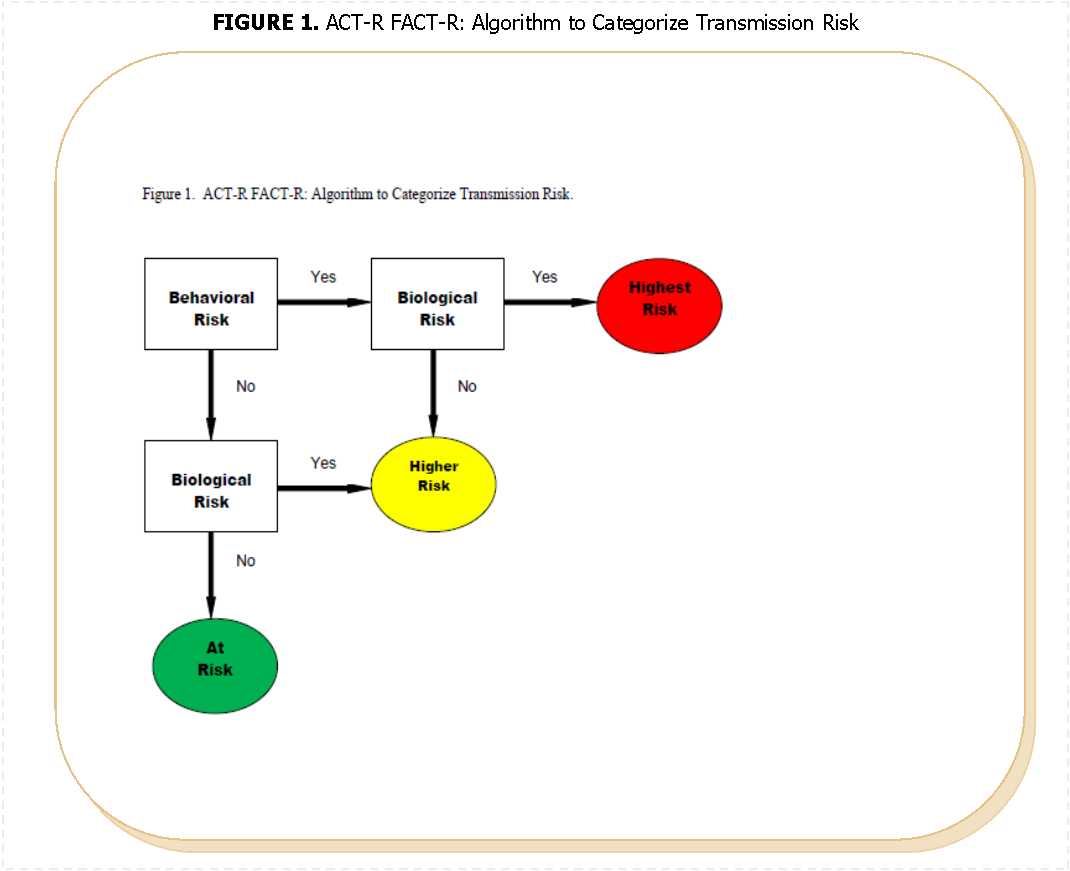
In conclusion, the Stages of Care continuum is very effective at simplifying a complex process of HIV clinical care. Reaching viral suppression requires a person know their HIV status (e.g. be tested and receive their results), then they must be linked to HIV care and present for their appointment (e.g. usually measured by at least 1 visit, or CD4/PVL count, within 12 months), then they must be retained in care (e.g. typically described as 2 visits, or CD4/PVL counts, within 12 months), then they must receive ART and adhere to their regimen, and then they must reach and maintain an undetectable viral load (e.g. <50 copies at last measurement). Most people with HIV are not virally suppressed. There is an urgent need to increase the number of HIV-infected people who achieve viral suppression. Review of the Stages of Care data show a linear decrease, or steady drop-off, through the stages. To reduce drop-offs, intervention strategies should be matched to a patient’s Stage of Care to help them transition to the next stage. We suggest that the ACT-R FACT-R or similar practical and easy-to-use clinical tools could be an effective stage-matched intervention for patients retained in care, but not yet on ART. Implementation of this tool in clinic settings could assist providers in their decisions to treat patients based on transmission risk, thereby providing an additional intervention that increases the proportion of HIV-infected individuals on ART. A considerable proportion of Americans that have initiated ART have been able to achieve viral suppression. Integrating stage-matched secondary prevention interventions into the treatment cascade may be a new way to help close the gap between key stages and further promote viral suppression for all.
(*when this study was conducted, treatment guidelines recommended initiation of ART based on CD4 count. However, there was growing evidence to support early initiation of therapy for secondary prevention and 2010 guidelines indicated a BIIa recommendation for those in serodiscordant relationships who did not qualify for initiation based on CD4 count9).
References
- 1.Hall H I, Frazier E L, Rhodes P. (2012) Continuum of HIV care: differences in care and treatment by sex and race/ethnicity. in the United States.Washington,DC,USA:XIX International AIDS Conference .
- 2.Cohen S M, Van Handel MM, Branson B M. (2011) Vital Signs: HIV prevention through care and treatment – United States. Morbidity and Mortality Weekly Reports. 60(47), 1618-1622.
- 3.Gardner E M, McLees M P, Steiner J F, del Rio C, Burman W J. (2011) The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clinical Infectious Diseases. 52(6), 793-800.
- 4.Department ofHealth and Human Services.Guidelines for the use of antiretroviral agents in HIV-1 infected adults and adolescents,updated(March29,2012).Retreived from www.aidsinfo.nih.gov.
- 5.Cohen M S, Chen Y Q, McCauley M. (2011) Prevention of HIV-1. , Infection with Early Antiretroviral Therapy N Engl J Med 365, 493-505.
- 6.Quinn T C, Wawer M J, Sewankambo N. (2000) Viral load and heterosexual transmission of human immunodeficiency virus type. , New England Journal of Medicine 342, 921-929.
- 7.Lally M A, O’Connell R, Peel S, Michael N, Jagodzinski L. (2008) Nucleic acid detection in patients whose HIV RNA levels are near the lower limit of detection:implications for endpoint determination in HIV vaccine trials.Boston,MA,USA: 15th Conference of Retroviral Opportunistic Infections.
- 8.Frater S C, Larson H E, Lally M A. (2011) Secondary prevention counseling among HIV-infected adults with detectable viral loads.Atlanta,GA,USA:. 2011National HIV Prevention Conference .
- 9.Thompson M A, Aberg J A, Cahn P. (2010) Antiretroviral treatment of adult HIV infection:. , recommendations of the International AIDS Society-USA panel. Journal of American Medical Association 304(3), 321-33.
- 10.Centers forDisease Control and Prevention. Incorporating HIV prevention into the medical care of persons living with HIV:. Recommendations of the CDC, the Health Resources and Services Administration, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Morbidity and Mortality Weekly Reports52(RR-12): 1-24.
