Demographics, Clinical Profile and Outcome among the HIV Infected Persons Hospitalized in the HAART Era in Barbados.
Abstract
Background:
HAART has resulted in significant decline in morbidity and mortality from HIV. However, it is unclear if the trends have continued in the current HAART era. An understanding of healthcare utilization patterns is important for optimization of care and resource allocation. We examined the diagnoses for hospitalizations of patients with HIV and their clinical and demographic profile years after the introduction of HAART.
Methods:
A retrospective audit of the HIV admissions from July 2009 through June 2010. The case notes of all the adult admissions where one of the discharge diagnoses was HIV infection was reviewed. Data including the demographics, date of diagnosis, treatment and the follow up details, admission outcome and the final diagnosis were extracted from the case notes.
Results:
Over the 12 months period there were 154 admissions where one of the discharge diagnosis was HIV infection, and this accounted for 2.9% of all medical admissions in adults. 103(67%) admissions were in persons who were known to be HIV infected prior to the current admission. HIV infection was diagnosed for the first time during the current admission in 51(33%) cases. Nearly two-thirds of those hospitalized, had a CD 4 cell counts of < 200/µL and 63 (66%) had a viral load greater than 50,000 copies/ml. Over all, opportunistic infection was the commonest (47%) discharge diagnosis, followed by serious bacterial infections and HIV nephropathy. The median duration of hospitalization was 6 days (Range 2 to 71 days). There were 49 (32%) deaths.
Conclusions:
A significant proportion of patients admitted with HIV infection were still diagnosed on admission and were found to be severely immunosuppressed. An opportunistic infection continues to be the commonest discharge diagnosis in HIV infected patients.
Author Contributions
Academic Editor: Larance Ronsard, National Institute of Immunology, New Delhi-110067.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2013 Alok Kumar,et.al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
The introduction of HAART has led to a decline in the overall hospitalizations rates as well as a reduction in the morbidity from the HIV infection 1, 2, 3, however, this decline has been unevenly distributed and inconsistent 4, 5, 6, 7, 8. There are reports that have noted a plateau effect or even an increased hospitalization due to relative increase in hospitalizations for non-HIV related reasons, such as drug toxicity, chronic liver disease, and non-HIV associated neoplasm 4, 5. It is clear that the interactions of morbidity, mortality, and hospitalizations due to HIV disease remain complex in the HAART era and may vary across various demographic and geographic groups. However, most reports of hospitalization from HIV infection in the HAART era are from the developed countries 1, 2, 3, 4, 5. There are very few published studies on HIV related hospitalization from the developing countries 9, 10, 11. All these reports from the developing countries are from settings where HAART was not used 9, 10, 11.
Barbados is one of the smaller countries in the English speaking Caribbean, with an estimated 2011 population of 286,705 and a 2010 estimated per capita gross national product of US$ 21,800. The adult prevalence rate of HIV in this country for 2011 is estimated at 1.4%, with the male: female ratio of 2:1 12. There is a provision for voluntary counseling and testing for HIV and an excellent facility for the follow up care and treatment of all HIV infected individuals in this country including provision for regular CD4 cell counts and Viral load estimation to follow the course of this illness and adjusting treatment. HAART is available free of cost for all HIV infected persons and it have been free since 2001. This country has made great progress in tackling this HIV epidemics over the past decade especially in the prevention of mother to child transmission of HIV and in the treatment of HIV infected persons after the introduction of HAART in early 2000 13, 14. We investigated all the hospital discharges in Barbados, where one of the discharge diagnoses was HIV/AIDS, to identify the causes of hospitalization among the HIV infected persons in the HAART era and to describe the profile of the hospitalized HIV infected persons.
Methods
This is a retrospective audit study during the period July 2009 through June 2010. This study was undertaken at the Queen Elizabeth Hospital (QEH). All adult (>16 years of age) admissions to the QEH where one of the discharge diagnose was recorded as HIV/AIDS were included in this study. Admissions for delivery in HIV infected persons were excluded from this study. The QEH is a tertiary level hospital with most modern investigative and therapeutic facilities and delivers over 95% of all inpatient care for its citizens in this country. It is a routine practice at the QEH to screen all adult inpatients on the medical wards for the HIV after counseling and patient consents. Ambulatory care and management of HIV infected persons in the country is coordinated and provided through a centralized HIV clinic the Ladymeade Reference Unit. Care and treatment including HAART has been available for the HIV infected persons in Barbados since 2002 at no direct cost at the point of delivery. Unique patient identification unit numbers are used to identify the cohort across both services and databases.
Adults who were hospitalized and where one of the discharge diagnoses was HIV/AIDS were identified from the central record department at the QEH. Medical records for all the hospitalized adult patients with HIV/AIDS were reviewed by one of the authors to extract the relevant data. Data collected included patient related information, history of drug abuse, self-described sexual orientation, date of diagnosis of HIV infection, CD4 counts and Viral load values at the time of the current admission and whether they received HAART prior to the current admission. Details of any prophylaxis against Pneumocystis jerovicii pneumonia (PJP) if received by the patient were also recorded. For persons who were on HAART at the time of current admission, duration of HAART and the adherence to the HAART regimen was recorded. Outcome of the current admission in term of discharge or death and the final diagnosis at the time of discharge or death was noted.
Outcome variables were the frequency and causes of hospitalization among HIV infected persons, duration of hospital stay, and endpoints of hospitalization in terms of death or discharge. Predictor variable includes- age, gender, CD4 cell counts and viral load values at the time of current hospitalization, and history of being on HAART. Bi-variate relationships between variables were investigated using the chi-square test of association for nominal variables. A 0.05 significance level was used for all statistical tests. For data management Microsoft Access, Microsoft Excel and SPSS version (10.1) were used. Necessary ethics approval was obtained from the ethics committee at the QEH.
Results
Over the 12 months period there were 154 adult (> 16 years) admissions to the QEH where one of the discharge diagnosis was HIV infection. A total of 148 adults were admitted. Four patients had more than one admission adding up to total of 154 admissions among the 148 adults. Admissions in HIV infected persons accounted for 2.9% (154/5279) of all medical admissions to the QEH. Table 1 show the characteristics of the HIV infected persons hospitalized during the study period. The median age at the time of hospitalization was 41 years (Range 16 – 71 years). Overall, 58% were males with the male to female ratio 1.4:1, 23% were men who had sex with men (MSM) and 22% smoked marijuana and/or cocaine. No patient reported intravenously drug abuse.
Table 1. Baseline characteristics of the HIV infected adults who were admitted during the study period.| Demographics | N | % |
| Age Group in Years (N=148) | ||
| 16-30 | 28 | (19) |
| 31-45 | 65 | (44) |
| 46-60 | 44 | (30) |
| > 60 | 10 | (7) |
| Gender (N=148) | ||
| Females | 62 | (42) |
| Males | 86 | (58) |
| Marital status (N=109) | ||
| Married | 26 (23.8) | |
| Unmarried | 83 (76.2) | |
| Self-Described Sexual orientation (N=98) | ||
| Heterosexual | 74 | (75) |
| Homosexual men | 12 | (12) |
| Bisexual men | 11 | (11) |
| Bisexual females | 1 | (1) |
| Drug abuse (N=93) | ||
| None | 73 | (78) |
| Marijuana smoking | 13 | (13) |
| Cocaine smoking | 7 | (8) |
| Intravenous drug abuse | 0 | (0) |
| Route of transmission (N=148) | ||
| Sexual | 146 (98.6) | |
| Perinatal | 1 (0.7) | |
| Blood transfusion | 1(0.7) |
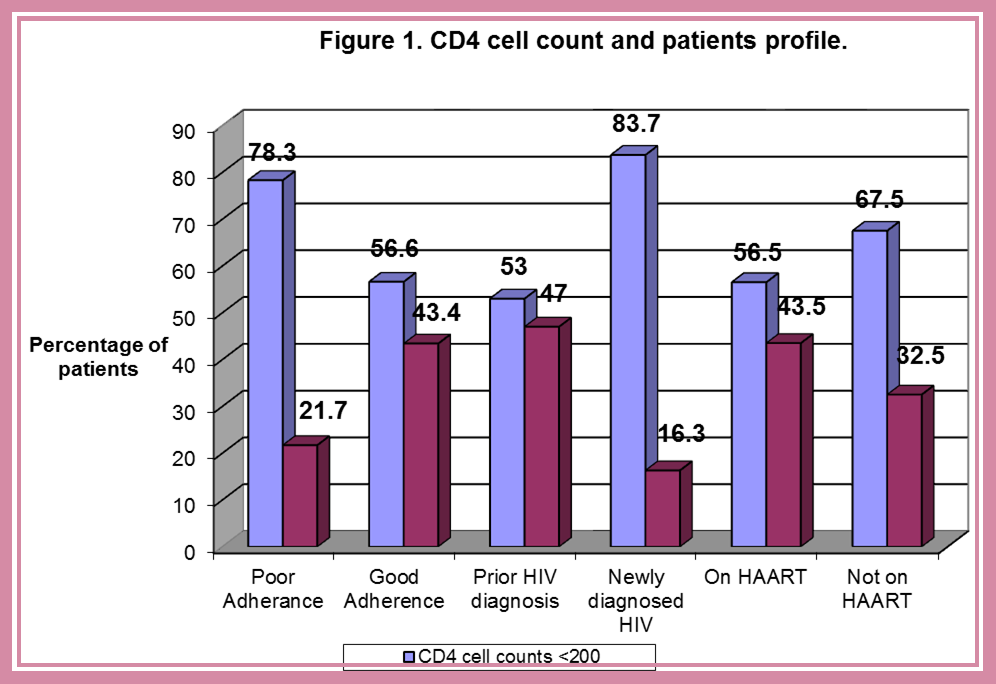
For those 103 patients known to be HIV infected at the time of their current hospitalization, median duration of time since their diagnosis was 31 months (Inter Quartile Range, 9 – 61 months) and 83(81%) had been receiving HAART treatment for a median duration of 10 months (Inter Quartile Range, 3 – 24 months). In 40(48%) of those on HAART, adherence was categorized as being poor (taking less than 90% of the prescribed medications). Twenty patients known to be HIV infected at the time of admission were not on HAART, 13 patients had defaulted from their follow up and 7 did not meet the criterion for starting HAART. (Figure 1). Thirty patients were on PJP prophylaxis with cotrimoxazole at appropriate recommended dose.
Figure 1.CD4 cell count and patients profile.
Of the 154 adults admissions to the QEH with the diagnosis of HIV/AIDS, 103 (67%) admissions were already known HIV infected, and the remaining 51(33%) of the hospitalizations were new cases diagnosed during the admission. Of those hospitalized and who had laboratory values recorded within 4 weeks of the time of admission 64% (51/81) had a CD 4 cell count of less than 200/µL. Among the 103 diagnosed HIV infected hospitalized patients who were known to be HIV infected prior to their admission, 47 had a CD4 cell counts done around the time of admission and 25 (53%) had a CD4 cell counts of <200/µL. Of the 51 admissions among the persons not known to be HIV infected prior to their admission, 34 had a CD4 cell counts done around the time of admission and 76% (26/34) had a CD4 cell counts <200/µL. This difference in the proportion of hiv infected persons based on their prior HIV status was statistically significant (Chi-square P= <0.0001) with an Odds Ratio of 4.65 (95% confidence interval 2.39, 9.03). A significantly higher proportion of persons with Poor adherence to HAART had a CD4 cell counts <200 (Chi-square P =0.0015, Odds Ratio =0.37; 95% CI 0.20, 0.69). However, the on Bivariate analysis correlation between the degree of adherence and the CD4 cell count was poor (Pearson Correlation r=0.37). Overall, 66% (65/96) of those who had a viral load measured had a value of over 50, 000 copies/ml Table 2. Among the 51 patients who were not known to be HIV infected prior to their admission, 29 had a viral load result and 21 (72%) had a value >50,000 copies/ml. Of the 103 patients known to be HIV infected at admission, 67 had a viral load done around the time of admission and 38 (57%) had a value >50,000 copies/ml. Among the 40 patients who were known to be HIV infected and were on HAART at the time of diagnosis and assessed to have poor adherence, 27 had a viral load study done around the time of admission and 21 (78%) had a value >50, 000 copies/ml.
Table 2. Clinical and laboratory characteristics of admissions.| N(%) | |
| CD4 cell count at admission (n=80) | |
| < 200/µL | 51 (64) |
| > 200/µL | 29 (36) |
| Viral load at admission (n=96) | |
| < 50 copies/ml | 10 (10) |
| 50 – 49999 copies/ml | 23 (24) |
| 50000 - 149999 copies/ml | 13 (14) |
| > 150000 copies/ml | 50 (52) |
| HIV diagnosis on admission (n=154) | |
| Known HIV+ | 103 (67) |
| Diagnosed during admission | 51 (33) |
| On HAART at admission (n=154) | |
| Known HIV+ on HAART | 83 (54) |
| Known HIV+ not on HAART | 20 (13) |
| New diagnosed | 51 (33) |
Over all, an opportunistic infection was one of the discharge/death diagnoses in 47%(63/154), followed by serious bacterial infections 13%(1//154) and HIV nephropathy 13%(N=17/154) Table 3. Common opportunistic infection as primary diagnosis included cerebral toxoplasmosis (N=31), PJP (N=14), Oropharyngeal candidiasis (N=7) disseminated herpes infection (N=5) and Cryptococcus meningitis (N=3). A non-HIV/AIDS-related condition was the primary final diagnosis in 21 cases of hospitalization (16%). Six admissions were for acute exacerbation of asthma, 5 for Diabetes Mellitus, two each for Dengue infection, suspected acute cardiac event and Sickle cell vaso-occlusive crisis, one each for status epilepticus, uncontrolled accelerated hypertension and suspected Leptospirosis. All these 21 admissions were among patients who were known to HIV infected at the time of admission and were on HAART.
Table 3. Primary discharge diagnosis for the HIV - related adult admissions to the QEH.| Table 3 Reason for admission (N=133)* | N(%) |
| Opportunistic infections | 63(47) |
| Serious bacterial infections | 17 (13) |
| Nephropathy | 17 (13) |
| Other AIDS related illness | 13 (10) |
| HAART toxicity | 2(1) |
| Non-AIDS related illness | 21(16) |
Median duration of the hospital stay was 6 days (Range, 2 – 37days). Over all, there were 25 deaths and 129 discharges over the one year study period. There were 12 deaths among persons not know to be HIV infected prior to their admission and 13 deaths among those known to be HIV infected prior to their current admission. Of the 13 deaths among persons known to be HIV infected prior to admission, 6 deaths were among those not on heart and 7 among those on HAART with all seven among those assessed to have poor adherence.
Discussion
In this study we found that the HIV-related hospitalizations continue to be a significant cause of medical admissions in adults. After the initial drop in hospitalization from HIV/AIDS following introduction of HAART, studies from both the developed and developing countries have also shown that hospitalization from HIV continues to be a significant public health problem 15, 16. The demographic of these HIV infected persons who were admitted is shown in Table 1.Over one-third of all the HIV related admissions were in persons not known to be HIV infected prior to this admission. Late diagnosis of HIV infection is common despite the universal availability of voluntary testing facility for HIV and anti-retroviral therapy to all Barbadian public free of cost at the point of delivery. Finding from the studies such as this one highlights the occurrence of late diagnosis of HIV in this country and should be used by health educators and counselors to encourage the general public for frequent and periodic testing for HIV on a voluntary basis.
Over all, nearly two-thirds of the adults admitted to the medical wards and who had HIV infection as one of the discharge diagnosis, had a CD4 cell count value < 200 and a viral load value of over 50,000copies/ml at the time of their admission. Both absence of prior diagnosis of HIV infection (newly diagnosed HIV infection) and absence of prior HAART was associated with significantly (P = 0.003) higher risk of having a CD4 cell counts <200 at the time of hospitalization These data are consistent with the fact that poor adherence to HAART and poor follow up with lack of HAART therapy are major problems in the HAART era and that this may offset the benefits of HAART in reducing the morbidity and mortality from HAART in this population.. Indirectly and perhaps more importantly, these findings highlight prevalence of high degree of stigma and discrimination prevalent in the society 17. The issue of stigma and discrimination of the HIV infected persons is further compounded by the mode of delivery of the health care and treatment for these people in this country. The centralized HIV/AIDS center which was meant to be the “one stop shop” for all the health care need of the HIV infected persons in this country may proving to be a double-edged sword, where by people may not be seen in a place popularly associated with the HIV care, in a small society such as this where practically everybody knows everybody else.
Consistent with the findings of a high proportion of the hospitalization occurring in newly diagnosed HIV infected individuals who were not on any HAART and who had a low CD4 cell count, opportunistic infection remains the single most frequent cause of HIV related hospitalization in this country in the era of HAART Table 3. Low CD4 counts, AIDS, and no current use of HAART are strongly correlated with hospitalizations especially those due to opportunistic infections 4, 7. What we also found is that a significant proportion of the adults with the prior diagnosis of HIV infection and who were hospitalized had severe immuno-supression with a CD4 cell counts <200/µL (36%) and over two-thirds of these patients were on HAART at the time of hospitalization. Poor adherence and emergence of resistance to the HAART regimen may be the possible reason for the immununologic failure in these patients on HAART. Nearly one-third of the patients on HAART were described to have poor adherence to the HAART regimen. Of those who had poor adherence, over 80% were on their third HAART regimen and all except one were on their second HAART regimen. After failing the first regimen which consisted of a combination of Combivir and Nevirapine, Nevirapine was empirically replaced by a protease inhibitor. No resistance testing was done in any of these patients. There are well controlled prospective study to show HIV related admissions from opportunistic infections occurred significantly more often in patients ignorant of their HIV status, those who did not have follow up and those that were non-compliant with their HAART 18. However, slow immune recovery could account for immuno-suppression in many patients 19.
There are some limitations to this retrospective observational study. Missing data were common, despite efforts to complete the data set. In particular, one third of patients were lacking viral load and CD4 T cell count data, and complete treatment data for the entire cohort are lacking. However, although, this is a hospital based study, this cohort of HIV infected persons requiring hospitalization is representative of the entire population of Barbados as QEH is the only hospital that provides inpatient care to the HIV infected persons in this country. This could be seen as strength of this study.
In conclusion, a significant proportion of patients admitted with HIV infection were the newly diagnosed and were more likely to be severely immuno-supressed with an increased risk for mortality. An opportunistic infection continues to be the commonest discharge diagnosis, although there was a growing trend in the proportion of the discharge diagnosis being Non-AIDS related conditions. Poor adherence to HAART or not being on HAART was associated with higher risk for death. Along with the existing problems of late diagnosis of the HIV infections and non-adherence to HAART, there is a growing trend toward increasing admissions for HAART toxicity and Non-AIDS related conditions. Also, as persons with AIDS on HAART are living longer, there is an increase in the nutritional problems such as anemia, and chronic diseases such as nephropathy.
References
- 1.Mocroft A, Monforte A, Kirk O, Johnson M A, Friis-Moller N et al.. (2004Nov) EuroSIDA study group. Changes in hospital admissions across Europe: 1995-2003. Results from the EuroSIDA study. HIV Med 5(6), 437-47.
- 2.Kumar A, Kilaru K R, Forde S.Roach TC.(2006)Changing HIV Infection-Related Mortality Rate and Causes. of Death among Persons with HIV Infection before and After the Introduction of Highly Active Antiretroviral Therapy:Analysis of All HIV-Related Deaths in Barbados,1997-2005.J.Int Assoc Physicians AIDS Care (Chic Ill) 5(3), 109-14.
- 3.Paul S, Gilbert H M, Lande L, Vaamonde C M, Jacobs J et al. (2002) Impact of antiretroviral therapy on decreasing hospitalization rates of HIV-infected patients in2001. AIDS Res Hum Retroviruses. 18(7), 501-6.
- 4.Gebo K A, Diener-West M, Moore R D.(2001Jun1) Hospitalization rates in an urban cohort after the introduction of highly active antiretroviral therapy. , J Acquir Immune Defic Syndr 27(2), 143-52.
- 5.Floris-Moore M, Lo Y, Klein R S, Budner N, Gourevitch M N et al.(Nov1,2003) Gender and hospitalization patterns among HIV-infected drug users before and after the availability of highly active antiretroviral therapy.J Acquir Immune Defic Syndr. 34(3), 331-7.
- 6.L H Thompson, Sochocki M, Friesen T.(April2012) Medical ward admissions among HIV-positive patients in Winnipeg. , Canada,2003–10 Int J STD AIDS 23, 287-288.
- 7.Krentz H B, Dean S, Gill M J.(2006Oct) Longitudinal assessment(1995-2003) of hospitalizations of HIV-infected patients within a geographical population in Canada. , HIV Med 7(7), 457-66.
- 8.Keiser P, Kvanli M B, Turner D, Reisch J, Smith J W et al.(Jan1,1999) Protease inhibitor-based therapy is associated with decreased HIV-related health care costs in men treated at a Veterans Administration hospital. J Acquir Immune Defic Syndr Hum Retrovirol. 20(1), 28-33.
- 9.Sok P, Harwell J I, McGarvey S T, Lurie M, Lynen L et al.(2006May)Demographic and clinical characteristics of HIV-infected inpatients and outpatients at a Cambodian hospital. , AIDS Patient Care STDS 20(5), 369-78.
- 10.Sharma S K, Kadhiravan T, Banga A, Goyal T, Bhatia I et al. (2004) (Nov22) Spectrum of clinical disease in a series of 135 hospitalised HIV-infected patients from north India. , BMC Infect Dis 4, 52.
- 11.Ogun S A, Adelowo O O, Familoni O B, Adefuye O B, Alebiosu C et al.(Oct2003) Spectrum and outcome of clinical diseases in adults living with AIDS at the Ogun State University Teaching Hospital. East Afr Med. , J 80(10), 513-7.
- 12.Caribbean Epidemeology Center/Pan American Health Organization/WHO. Status and trends:. epidemic1982-2002.CAREC Publication2004 , Analysis of the Caribbean HIV/AIDS
- 13.St John AM, Kumar A, Cave C.(May2003) Reduction in perinatal transmission and mortality from human immunodeficiency virus after intervention with zidovudine in Barbados. Pediatr Infect Dis. , J 22(5), 422-6.
- 14.Kilaru K R, Kumar A, Sippy N, Carter A O, Roach T C.(Mar2006) Immunological and virological responses to highly active antiretroviral therapy in a non-clinical trial setting in a developing Caribbean country. , HIV Med 7(2), 99-104.
- 15.Nancy F, Crum-Cianflone MPH, Grandits Greg, Echols Sara, Anuradha Ganesan RN et al. (2010) . the Infectious Disease Clinical Research Program. Trends and Causes of Hospitalizations among HIV-infected Persons during the Late HAART Era: What is the Impact of CD4 Counts and HAART Use? J Acquir Immune Defic Syndr 54(3), 248-257.
- 16.Ogoina Dimie, Reginald O Obiako, Haruna M Muktar. (2012) Morbidity and Mortality Patterns of Hospitalised Adult HIV/AIDS Patients in the Era of Highly Active Antiretroviral Therapy: A 4-year Retrospective Review from Zaria. , Northern Nigeria,”, AIDS Research and Treatment,vol.ArticleID 940580, 2012-10.
- 17.Rutledge S E, Abell N. (2005) Awareness, acceptance, and action: An emerging framework for understanding AIDS stigmatizing attitudes among community leaders in Barbados. AIDS Patient Care and STDs 19(3), 186-199.