Integrating Analgesic Doses and Pain Trend Analysis: A Novel Clinical Support System
Abstract
Background
Prescribing appropriate analgesics with optimal dosages based on patients' pain severity is challenging, especially when multiple painkillers are involved. Tracking and analyzing the effectiveness of analgesics and their dosages over time is crucial for pain management. Existing systems lack the ability to integrate analgesic equivalent doses with temporal trends in pain scores, hindering effective decision-making.
Methods
We developed a Clinical Support System that calculates the daily oral morphine equivalent dose and analyzes trends in consumed equivalent doses of analgesics. The system provides a graphical user interface that displays medication prescriptions, actual medication usage, and pain scores. It offers features such as correlating analgesic drug usage with pain intensity, trend analysis of analgesic drug usage and pain intensity, and identification of effective oral morphine equivalent doses.
Results
The system overcomes previous barriers in drug analysis by providing real-time calculation of oral morphine equivalents and trend analysis of pain duration. It assists physicians in prescribing appropriate and safe medication dosages, enhancing medication safety for patients.
Conclusions
Our clinical support system offers a comprehensive solution for analyzing trends in consumed equivalent doses of analgesics. It integrates medication prescriptions, actual usage, and pain scores, providing decision-making support for pain management.
Author Contributions
Copyright © 2025 Shih Chieh Yang, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Patients’ perception of pain is subjective. It has always been complicated to prescribe advisable analgesics with optimal dosages according to a patient’s pain severity, especially when the patient has been prescribed a variety of painkillers 1. Thus, it is vitally important to establish the effective relative doses of individual analgesics using data from doctors’ orders, in order to determine whether or not to change the analgesics or adjust the doses of the individual analgesics in the following days 2.
Patients often have difficulty identifying which analgesic provides effective relief of their pain, especially when the medication orders change frequently due to unsatisfactory pain control 3. It is also challenging for patients to differentiate between regular medication administration and “pro re nata” medication when experiencing acute pain. Hence physicians need to cross-reference the patient's description with each dose of medication. It is necessary to compare the administration time with the corresponding pain score changes in order to obtain more empirical evidence. If we solely rely on prescriptions without simultaneously considering the pain scores, it is not possible to determine which medication was effective. Additionally, patients often receive various analgesics concurrently, which makes long-term tracking more challenging 4.
Calculating the daily oral morphine equivalent dose is already difficult, and comparing it over multiple days poses an even greater challenge. When combining the patient's pain scores, many existing systems cannot immediately show how temporal trends in pain scores change with different drugs 5. Clinicians may need to update orders and prescriptions frequently, but if there are multiple analgesics, they may inadvertently neglect to check whether the prescriptions and doses are correct. Many medication prescriptions have set start and end dates, especially for high-risk drugs or various opioid medications. Therefore, a situation may arise in which the physician is unaware that a patient’s medication has reached its end date, resulting in the patient being without adequate pain relief. Moreover, we also have to consider whether the daily oral morphine equivalent dose is sufficient. Both overdosing or underdosing can directly impact patient safety 6. Some systems provide clear information in individual timeframes, but data over an extended period are not easily interpretable and are more difficult to understand. Patients with chronic pain typically use multiple analgesics, and therefore it becomes challenging to comprehensively understand the quantities of medications 7.
To date, there is no optimal system that can effectively analyze and integrate analgesic equivalent doses with trends to provide decision-making support for adjustment of analgesics and their doses. Moreover, there is no optimized user interface that can provide integrated information.
In the past, many systems were only able to check medications at single or multiple time points, but they could not provide the equivalent dose at a glance. For example, there are various types of opioid-like medications, and each type has a different strength, typically represented in terms of Morphine Milligram Equivalents (MME) for oral morphine equivalence 8. For any given medication, different routes of administration and formulations may have varying oral morphine equivalents 9. Moreover, medications can be given in fractions or varying doses, such as half a tablet, half a syringe, or a quarter of a syringe. A patient may receive multiple different medications simultaneously, and each doctor may have a different perspective on the weighting of these medications 10. As a result, calculating the daily oral morphine equivalent dose can be challenging.
Therefore, we devised a system that not only provides addictive doses for different opioids but also offers information on other analgesics, which can help doctors in the management of different kinds of pain.
Methods
Morphine Milligram Equivalents
The system that we developed can instantly calculate the oral morphine equivalent doses (Morphine Milligram Equivalents (MME)) of various opioids (Opioids) actually administered in the past 8-72 hours. The system can further provide the analysis setting by layout design to provide the time trend of the relative pain intensity with its oral morphine equivalent dose from different time points, and can also add the trend of other auxiliary drugs (including anti-inflammatory analgesics, muscle relaxants, related neuropathic analgesics) prescribed by the doctors and taken by the patients (Figure 1).
Figure 1.Morphine Milligram Equivalents dashboard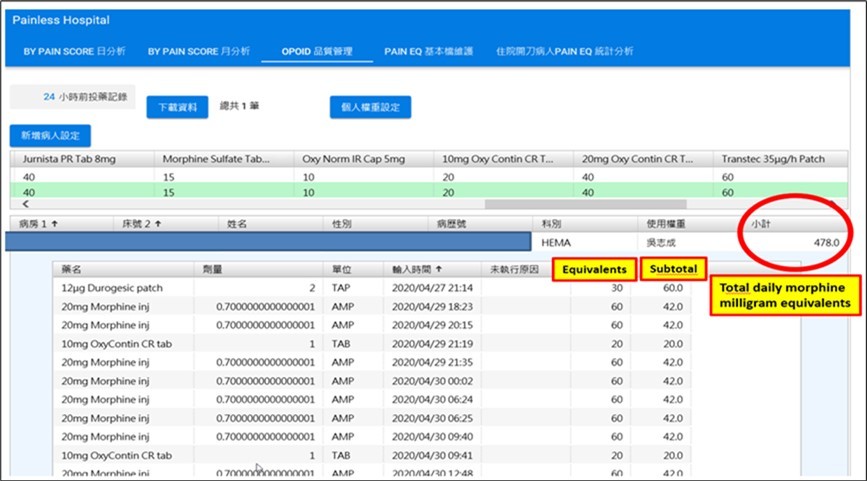
This tool takes physician preferences and individual patient differences into consideration, and allows the user to adjust weight conversions accordingly. It offers three modes: (a) Default values (unchangeable) (Table 1), (b) Physician's own settings (once modified, these conversion weights will be applied to all patients when logged in), and (c) Patient-specific settings (once modified, only this patient will have these conversion weights applied). The priority order for weight settings is (c) > (b) > (a) (Table 2).
Table 1. Equianalgesic dosing table for opioids (Default)| Drug Weight Conversion Table | |
|---|---|
| Drug Name | Weight |
| 75 ug durogesic patch | 180 |
| 500ug/10ml fentanyl | 150 |
| 25 ug durogesic patch | 60 |
| 50 ug durogesic patch | 120 |
| 12ug durogesic patch | 30 |
| 100ug/2ml fentanyl inj | 30 |
| morphine inj 10mg | 30 |
| 30mg Morphine tab | 30 |
| 20mg morphine inj | 60 |
| XL morphine-60 cap | 60 |
| Jurnista PR tab 8mg | 40 |
| Morphine sulfate tab 15mg | 15 |
| Oxynorm IR cap 5 mg | 10 |
| 10mg OxyContin Cap | 20 |
| 20mg OxyContin Cap | 40 |
| Type | 75ug Durogesic Patch | 500mcg 10mL Fentany L inj PPCD | 25ug Fentany Patch | 50ug Fentany L Patch | 12pg Durogesic Patch |
| Default | 180 | 150 | 60 | 120 | 30 |
| Physician’s settings | 180 | 150 | 60 | 120 | 30 |
| 100mcg/2mL Fentany Linj | Morphine in 10mg | 30mg Morphine Tab | 20mg Morphine inj | XL Morphine 60 Cap | Jumista PR Tab Img |
| 30 | 30 | 30 | 60 | 60 | 40 |
| 30 | 30 | 30 | 60 | 60 | 40 |
| XL Morphine 60 Cap | Jumista PR Tab 8mg | Morphine Sulfate Tab 1 | Cary Norm R Cap 5mg | 10mg Only Contin CR Tab | 20mg Oxy Contin CR Tab |
| 60 | 40 | 15 | 10 | 20 | 40 |
| 60 | 40 | 15 | 10 | 20 | 40 |
Graphic user interface GUI
The system provides a user-friendly graphic display, and when used in conjunction with pain scores, prescriptions, and actual consumption of various analgesic drugs, it can provide medical staff with a more accurate reference for clinical decision-making with respect to various prescriptions for analgesics.
With the assistance of a user-friendly graphical interface, our system simplifies the tracking of patients' medication prescriptions and actual usage history (Figure 2). It provides a chronological representation of past, present, and future medication usage, offering an analysis of trends related to daily administered Morphine Milligram Equivalents (MME) of oral morphine equivalents and pain scores (Figure 3). The system provides the following information:
Figure 2.Graphic user interface of patients' medication prescriptions and actual usage history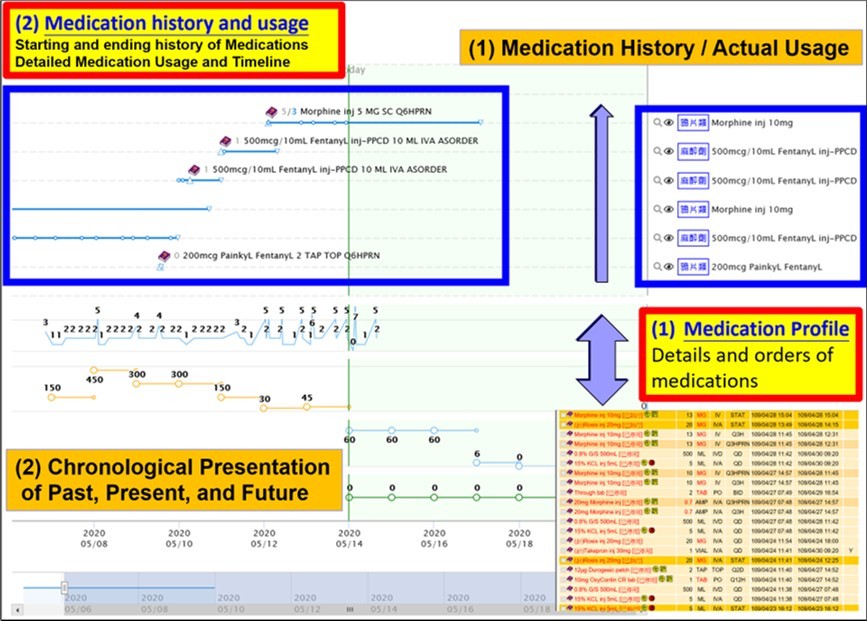
Figure 3.Chronological representation of medication usage, offering a trend analysis of the daily administered Morphine Milligram Equivalents (MME) of oral morphine equivalents in relation to pain scores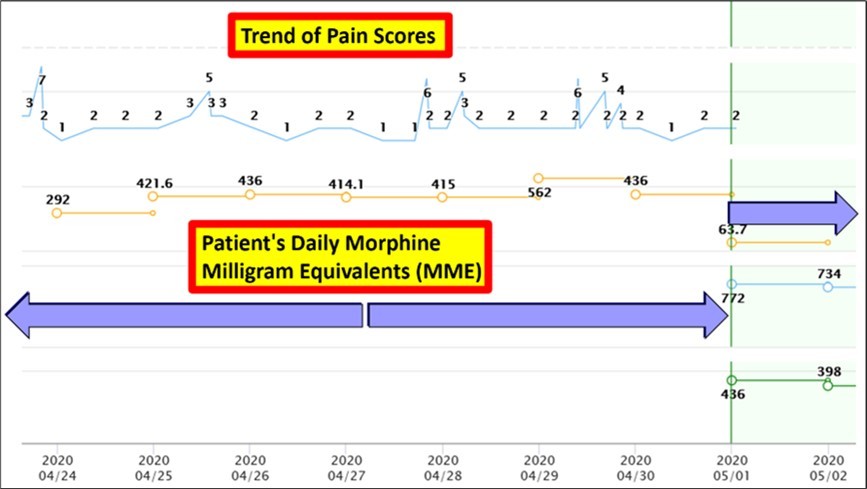
Information on the correlation between analgesic drug usage and pain intensity, making it easy to identify which medications are effective (Figure 4).
Figure 4.Intuitive presentation of correlation between pain score changes and medication usage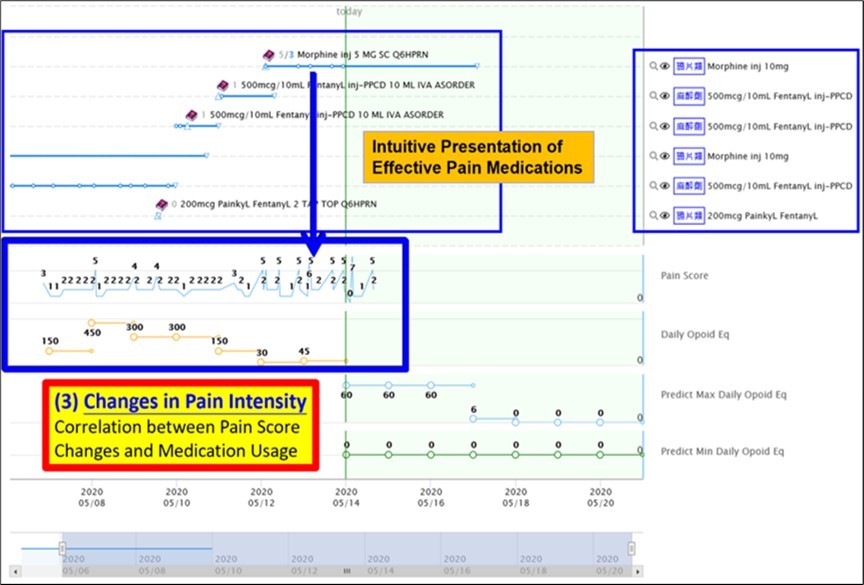
Information on the trend of analgesic drug usage and pain intensity, facilitating the analysis of the relationship between oral morphine equivalent doses and pain over time (Figure 5).
Figure 5.Trend of the relationship between oral morphine equivalent doses and pain over time
Daily consumption of morphine medication equivalents by the patient, enabling identification of the effective oral morphine equivalent dose based on the displayed pain scores.
Analysis of the contribution of various opioids to the oral morphine equivalent dose.
The combined effects of medications are displayed on the screen, allowing for visual assessment and long-term monitoring.
Identification of the highest and lowest prescribed oral morphine equivalent doses, in conjunction with the known effective oral morphine equivalent dose for the patient, facilitating the evaluation of the rationale for and appropriateness of future analgesic prescriptions (Figure 6).
Figure 6.Identification of the highest and lowest prescribed oral morphine equivalent doses and prediction of appropriate future MME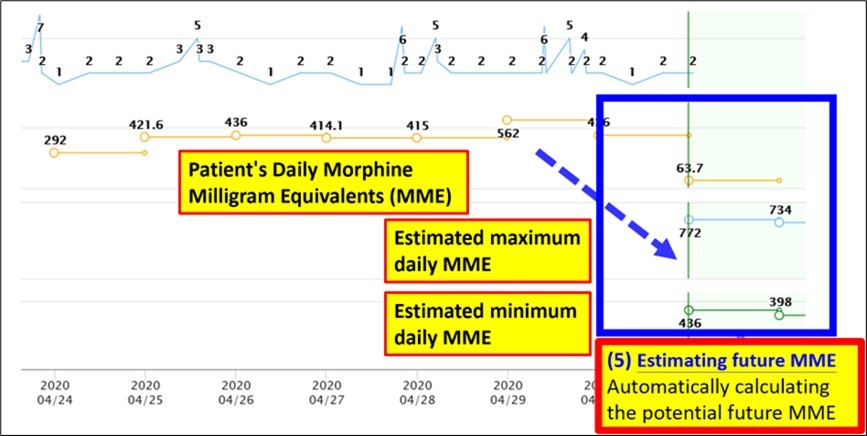
Line graph displaying the start and end dates of medications (including markers and values), serving as a reminder of the timing of future analgesic prescriptions (Figure 7).
Figure 7.Line graph showing the start and end dates of medications, serving as a reminder for the timing of future analgesic prescriptions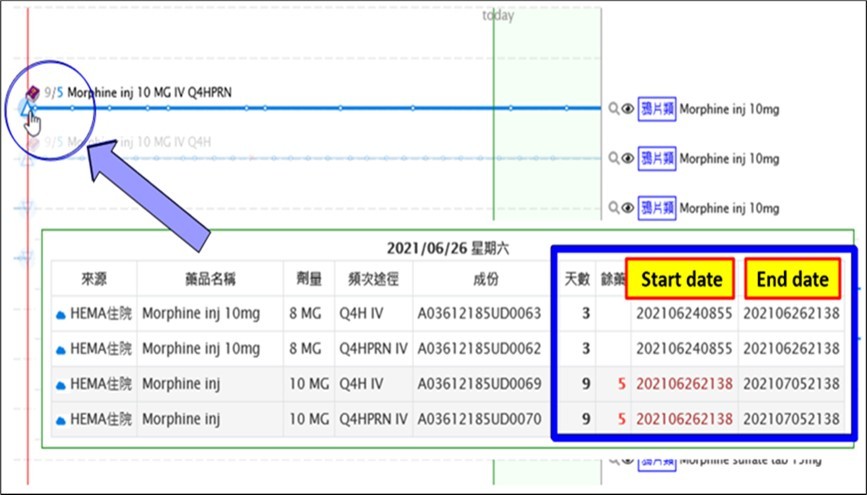
Technological maturity
The Pain Management System has undergone clinical validation in our hospital since December 2017. It was implemented in our medical system in July 2018, along with the activation of a hospital-wide opioid equivalent dose calculation dashboard. Clinical validation was completed in April 2019, and the system has been verified for practical use in clinical settings.
This system is specifically designed to provide support for clinical treatment and can be integrated with other interfaces as needed. It directly captures patients' actual usage records without the need for manual queries or input, reducing the risk of missing information or human input errors. The system does not require separate initiation, making it more adaptable to clinical requirements and providing real-time analysis. It has the potential to become an essential tool for assisting physicians in prescribing pain medication and tracking the effectiveness of pain management interventions in the future.
Intellectual Property Protection Strategies and Advantages
This system has obtained a new patent in Taiwan. The related research and development were conducted at our hospital's Clinical Informatics Center, and the technical documents and testing processes are stored within the hospital. Currently, the system operates in the hospital through a connected application programming interface (API), ensuring there are no concerns regarding technology leakage.
Results
Integration of Pain Relief Effectiveness and Prediction
Because the system provides addictive doses for different opioids as well as information on other analgesics, it is capable of assisting doctors in the management of different kinds of pain. This system overcomes previous barriers in drug analysis by enabling real-time calculation of oral morphine equivalents and providing analysis of the relative equivalents and trends in pain duration. It assists physicians in prescribing appropriate and safe medication dosages, saving time and enhancing medication safety for patients.
Application Value and Benefits
The interface design of this system effectively integrates the following information: (a) Medication prescribing (for doctors), (b) Actual medication consumption (for patients), and (c) Pain trend analysis (pain relief effectiveness), to provide efficient decision support (Table 3).
Table 3. Comparison between our clinical support system and typical hospital systems| Our Clinical Support System | Typical hospital systems | |
| Integrated interface | Graphic user interface | - |
| Checking medication history | Automatic/real-time | Manual/time-consuming/error-prone |
| Correlation between pain score and medication | Intuitive/easy to interpret | Not ideal |
| Medication equivalent calculation | Automatic/real-time | Manual/time-consuming/error-prone |
| Prediction of future MME | Automatic/real-time | - |
Discussion
There has been no similar or comparable system in the past that effectively integrates the trend analysis of pain medication consumption, and to date there has been no optimal interface design capable of providing integrated information. In addition to its various clinical applications, our system can contribute in other areas.
In terms of clinical education, this system can expand the evaluation of pain treatment effectiveness from a single time point score to the combined presentation of pain scores over time, medication response, and trend analysis. This expansion from text-based teaching to graphical representation can make pain education more engaging and relatable. Medical data digitization is the gateway to intelligent healthcare, and the use of systems that analyze pain trends and their relationship medication dosages paves the way for further development of smart tools in pain management11.
In medical applications, the quantification and graphical representation can be applied to other medical disciplines as well. After customization, this system can systematically present information on the relationships between corticosteroids and inflammation indices in immunology and rheumatology, targeted therapy and tumor indices in oncology, and immunosuppressants and renal function in nephrology.
For medication applications, the system allows analyses of drug efficacy assessments based on actual responses taking into account variations in medication, dosage, and patient indices. It is worth keeping in mind that the response of individual patients to any given medication varies in terms of drug interactions, metabolism, and excretion. The establishment of personalized dose-response curves of drugs would provide actual utility in clinical practice 12.
In terms of future applications, our system can be expanded to include apps on patients’ smartphones or tablets. Apps can provide patients with access to the hospital's medication prescribing information, with seamless integration of medication use and pain scores. The hospital can provide medication information via a mobile app, which can remind patients when to take a medication and allow them to indicate if they have already taken it. The app can also provide a platform for patients to record their pain scores, which can be sent back to the hospital's system for analysis by healthcare professionals. The doctors can assess the effectiveness of medications and provide recommendations simultaneously. If the patient is hospitalized, the integration of medication use and pain score recording can also be achieved. In addition to enhancing the quality of pain management, the system can also increase patients’ engagement and adherence to the hospital's services.
Conclusion
Our clinical support system addresses the complexities and challenges associated with prescribing and tracking analgesic medications for patients. By integrating real-time calculations of oral morphine equivalents and providing comprehensive analyses of pain duration trends, the system offers physicians valuable decision-making support. It overcomes previous barriers in drug analysis by taking multiple analgesics into account, including opioids and other auxiliary drugs. It has the potential to revolutionize pain management practices and enhance patient outcomes.
References
- 1.Phillips J K, Ford M A, Bonnie R J. (2017) Pain management and the opioid epidemic: balancing societal and individual benefits and risks of prescription opioid use. National Academies of Sciences. National Academies Press (US). ISBN-13: 978-0.
- 2.Schneider C, Yale S H, Larson M. (2003) Principles of pain management. Clin Med Res. 1(4), 337-40.
- 3.Whitten C E, Evans C M, Cristobal K. (2005) Pain management doesn’t have to be a pain: working and communicating effectively with patients who have chronic pain. , Perm J 9(2), 41-8.
- 4.Breivik H, Borchgrevink P C, Allen S M, Rosseland L A, Romundstad L et al. (2008) Assessment of pain. , Br J Anaesth 101-17.
- 5.Milani D A Queremel, D. Pain Management Medications, StatPearls Publishing, Treasure Island (FL) (2020) .
- 6.Tariq R A, Vashisht R, Sinha A. (2020) Medication Dispensing Errors and Prevention. In: StatPearls StatPearls Publishing.
- 7.Adesoye A, Duncan N. (2017) Acute pain management in patients with opioid tolerance. , US Pharmacist 42, 28-32.
- 8.J A Lossio-Ventura, Song W, Sainlaire M, P C Dykes, Hernandez-Boussard T. (2022) Opioid2MME: Standardizing opioid prescriptions to morphine milligram equivalents from electronic health records. , Int. J. Med. Inf 162.
- 9.Drewes A M, Jensen R D, Nielsen L M. (2013) Differences between opioids: pharmacological, experimental, clinical and economical perspectives. , Br J Clin Pharmacol 75, 60-78.
- 10.G T Owen, B M, C M Schade, M S Eckmann, E C Hustak et al. (2018) Evidence-based pain medicine for primary care physicians. , Proc. (Baylor Univ. Med. Cent.) 31(1), 37-47.
