The Tinged Parchment-Cutaneous Mastocytosis
Abstract
A clinical image and brief discussion of cutaneous mastocytosis describe presentation, dermoscopy, and diagnostic clues. The note underscores when to evaluate for systemic involvement.
Author Contributions
Academic Editor: Ian James Martins, Director Edith Cowan University
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2023 Anubha Bajaj.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Mastocytosis is configured of monomorphic population of atypical mast cells admixed with a minimalistic population of eosinophils. Cutaneous mastocytosis is a frequently discerned mast cell disorder. Urticaria pigmentosa is a commonly discerned variant of mastocytosis exemplifying innumerable miniature, yellow brown papules which convert into hives upon abrasion.
Telangiectasia macularis eruptive perstans (TMEP) is a condition delineating light brown or dark brown cutaneous macules associated with telangiectasia. Previously designated as urticaria pigmentosa, maculopapular cutaneous mastocytosis is a frequently delineated variant occurring within adults or paediatric subjects.
Cutaneous mastocytosis may emerge at birth or during initial three months of infant life. Lesions are associated with flushing attacks on account of elevated content of histamine. Lesions may frequently undergo spontaneous involution. Cutaneous mastocytosis is associated with genomic mutations within CD117 gene1, 2. Urticaria pigmentosa is a frequently exemplified variant of cutaneous mastocytosis. Disease onset occurs within childhood. Lesions are comprised of multiple, brown macules 1, 2. Systemic variant of urticaria pigmentosa is a malignant condition incriminating hepatic parenchyma, spleen, bone marrow or lymph nodes. Occasionally, peripheral blood may depict circulating mast cells with the configuration of mast cell leukaemia 1, 2. Cutaneous mastocytosis may articulate a solitary lesion or delineate an accumulation of miniature lesions configuring urticaria pigmentosa. The condition commonly incriminates extremities and trunk whereas palms and soles are spared 3, 4. Generally, red, brown, pink or yellow nodules or plaques of up to 1.0 centimetre magnitude may be observed. Lesions tend to blister. Upon microscopy, mast cells configuring macules and plaques appear preponderantly confined within papillary dermis. Mast cells emerge as spherical to spindle shaped cells permeated with abundant, eosinophilic cytoplasm, distinctive cytoplasmic boundaries and enlarged, pale nuclei. Mast cells are frequently admixed with a reactive inflammatory cell exudate comprised of eosinophils. Besides, accompanying oedema appears confined to papillary dermis. Vesicles may be configured within sub epidermal zone 3, 4. Upon microscopy, maculopapular cutaneous mastocytosis demonstrates accumulation of mast cells confined within the dermis. Mast cells appear as spherical or spindle shaped cells incorporated with abundant, eosinophilic cytoplasm demonstrating minute granules, distinct cytoplasmic boundaries and enlarged, pale nuclei. Mast cells are commingled with diverse inflammatory cells as histiocytes, eosinophils, and lymphocytes. Traumatised lesions are accompanied by oedema of subjacent dermis 3, 4. Bullous mastocytosis can be appropriately discerned with Tzanck smear wherein accompanying inflammatory infiltrate is minimal and predominantly confined to perivascular region 3, 4.
Telangiectasia macularis eruptive perstans demonstrates subtle microscopic features with elevated mast cells circumscribing distended superficial capillaries. Mast cell aggregates appear admixed with superficially disseminated lymphoid and histiocytic inflammatory infiltrate. Superimposed epidermal layer exhibits hyperpigmentation of basal cell layer3, 4.
Mast cells configuring lesions of maculopapular cutaneous mastocytosis can be highlighted with specific Darier's sign is constituted of a ‘stroking skin’ which releases histamine with the generation of hives. Dermatographism is constituted of dermal oedema simulating hives, a feature which arises due to stroking the cutaneous surface with a pointed instrument. stains as Giemsa, toluidine blue, tryptase or Leder’s special chloroacetate esterase stain. Toluidine blue and Giemsa demonstrate metachromasia within mast cells wherein granules appear purple red. Mast cells appear immune reactive to CD117 (c-KIT) 6, 7.(Table 1)(Table 2)(Figure 1)(Figure 2)
Figure 1.Cutaneous mastocytosis demonstrating a dermal infiltrate of atypical mast cells imbued with abundant, eosinophilic cytoplasm, minute granules and enlarged, pale nuclei. Mast cells appear intermixed with reactive inflammatory cells as histiocytes, lymphocytes and eosinophils. Stratified squamous epithelium is superimposed upon mast cell aggregates(8).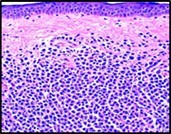
Figure 2.Cutaneous mastocytosis enunciating aggregates of atypical, spherical mast cells incorporated with abundant, eosinophilic cytoplasm, few basophilic granules and enlarged pale nuclei. The mast cell infiltrate is commingled with reactive inflammatory cells and vascular articulations. Stratified squamous epithelium is superimposed upon accumulated mast cells(9).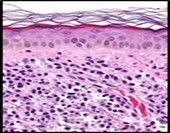
| •cutaneous mastocytosis |
| ~maculopapular cutaneous mastocytosis(urticarial pigmentosa) |
| ~diffuse cutaneous mastocytosis |
| ~mastocytoma of skin |
| •systemic mastocytosis |
| ~indolent systemic mastocytosis |
| ~smouldering systemic mastocytosis |
| ~systemic mastocytosis with associated haematological neoplasm or systemic mastocytosis associated with clonal hematologic non mast cell lineage disease |
| ~aggressive systemic mastocytosis |
| ~mast cell leukaemia |
| •mast cell sarcoma |
| Variant | Diagnostic criterion |
|---|---|
| Maculopapular cutaneous mastocytosis | Typically pigmented cutaneous lesions. Darier’s sign+. |
| Urticaria pigmentosa | Confirmatory histology. KIT mutation in lesional skin. |
| ~monomorphic variant | Monomorphic cutaneous lesions |
| ~polymorphic variant | Polymorphic cutaneous lesions. Absent features of systemic mastocytosis. |
| Diffuse cutaneous mastocytosis | Confirmatory histology. Darier’s sign+. Incrimination of entire cutaneous surface. Absent features of systemic mastocytosis |
| Cutaneous mastocytoma | Confirmatory histology. Darier’s sign+ |
| ~isolated mastocytoma | Singular lesion |
| ~multi-localized mastocytoma | Multiple (2 to 3) lesions. Absent features of systemic mastocytosis |
Cutaneous mastocytosis requires segregation from normal cutaneous surfaces or conditions such as dermatosis, chronic dermatitis, nodular prurigo, venous stasis, bullous impetigo, urticaria, juvenile xanthogranuloma, arthropod stings or autoimmune bullous diseases 6, 7.
Maculopapular cutaneous mastocytosis necessitates distinction from Langerhans cell histiocytosis or urticarial 6, 7.
Cutaneous mastocytosis can be appropriately managed with symptomatic therapy. Topical agents as calcineurin inhibitors or corticosteroids may be optimally adopted to treat the condition. Efficacious systemic therapy is preponderantly comprised of oral antihistamines. Besides, agents such as oral cromolyn sodium, oral corticosteroids, omalizumab, oral psoralen and ultraviolet A(PUVA), narrowband ultraviolet B or ultraviolet A1(UVA1) radiation may be beneficially employed 6, 7. Urticaria pigmentosa can be suitably managed with a pre-measured epinephrine pen with auto-injector. Circumvention of possible disease trigger mechanisms is necessitated 6, 7. Spontaneous retrogression of maculopapular mastocytosis within adults is uncommon.
The cutaneous variant may exceptionally engender systemic mastocytosis with dissemination into >singular soft tissue sites.
Cutaneous mastocytosis is associated with superior prognostic outcomes 6, 7.
References
- 2.Leru P M. (2022) Evaluation and Classification of Mast Cell Disorders: A Difficult to Manage Pathology in Clinical Practice. Cureus. 14-2.
- 3.Leguit R J, Wang S A, George T I. (2022) The international consensus classification of mastocytosis and related entities. Virchows Arch. 10-1007.
- 4.Macri A, Pigmentosa Cook C Urticaria. Stat Pearls International (2022) . , Treasure Island, Florida
- 5.Valent P, Akin C, Hartmann K. (2017) Advances in the Classification and Treatment of Mastocytosis: Current Status and Outlook toward the Future. Cancer Res. 77(6), 1261-1270.
